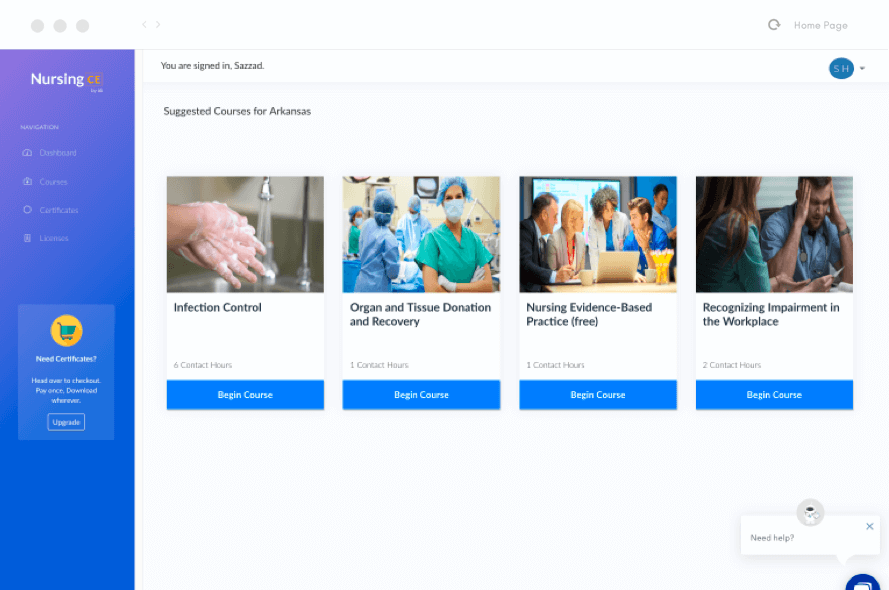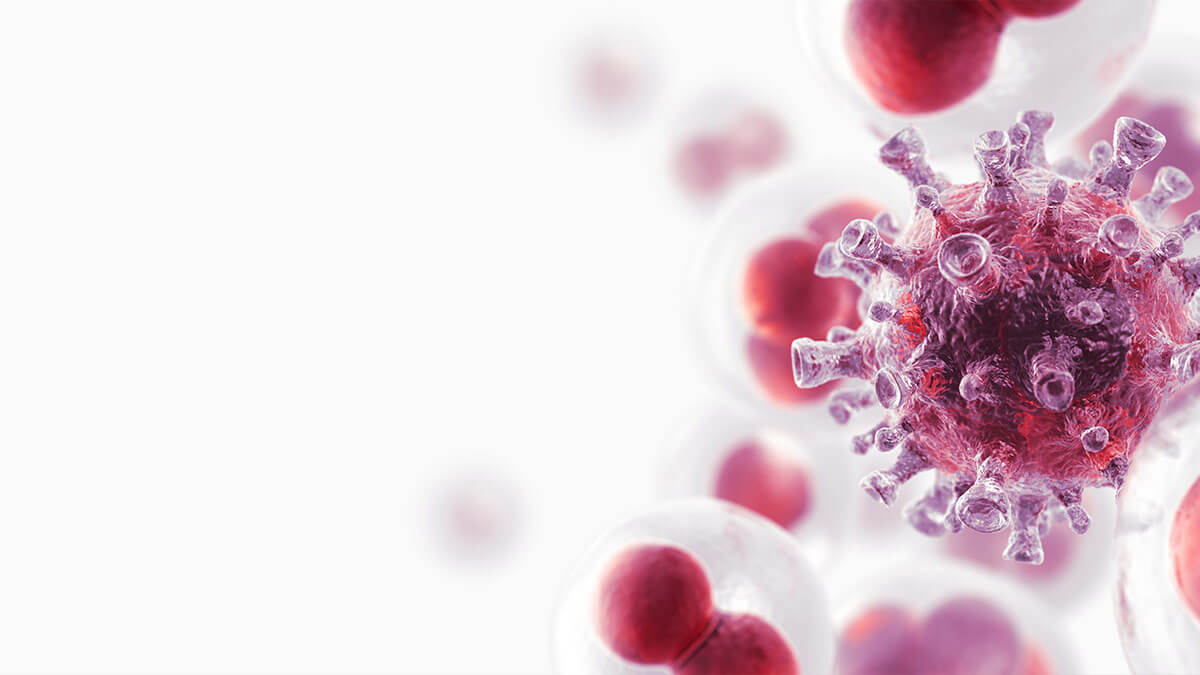
Oncology Medication Administration Nursing CE Course for RNs and LPNs
This course provides an overview of the various oral and intravenous (IV) cancer treatment modalities, including chemotherapy, targeted agents, biological and immune-mediated therapies, hormonal treatments, and chemoprevention.