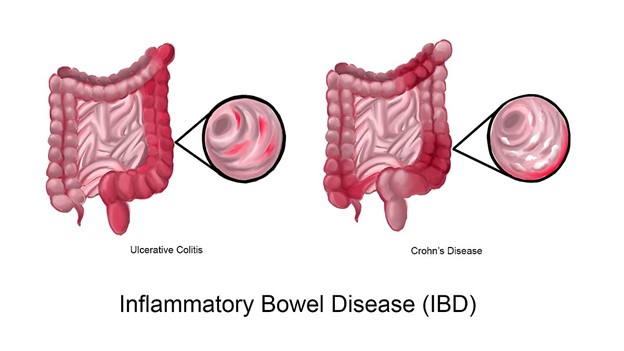
This learning activity aims to increase advanced practice registered nurses' (APRNs') knowledge of inflammatory bowel disease (IBD), including the difference between ulcerative colitis and Crohn's disease. This includes the pathophysiology, clinical manifestations, risk factors, diagnostic testing, and treatment options for both types of IBD.
...purchase below to continue the course
d infiltration of cytokines that activate neutrophils, plasma cells, lymphocytes, macrophages, mast cells, and eosinophils. When macrophages are activated, they can lead to the presence of cytokines that cause fever during the acute phase of ulcerative colitis. The resulting inflammation damages the intestinal wall's mucosal barrier, which allows fluid to leak into the gut (McCance & Huether, 2019).
The mucosa can become hyperemic and edematous when mild inflammation is present, leading to a dark red and velvety appearance. The mucosa becomes hemorrhagic with small erosions that merge into ulcers if inflammation is severe. Abscesses can form in the crypts, and granulation tissue can develop due to necrosis and ulceration of the mucosa. Edema and thickening of the muscularis mucosa can lead to a narrowing of the affected colon. With chronic disease, inflammatory polyps may develop over time due to the rapidly regenerating epithelium (McCance & Huether, 2019). Figure 2 depicts the anatomy of the GI tract.
Figure 2
Layers of the GI Tract

(Goran tek-en, 2014)
Risk Factors
There are many risk factors specific to ulcerative colitis. Some of the risk factors are modifiable, while others are nonmodifiable. Examples of the risk factors for the development of ulcerative colitis include:
- family history: this is the most critical risk factor and accounts for 8% to 14% of patients diagnosed with ulcerative colitis; individuals with a 1st-degree relative diagnosed with ulcerative colitis were four times more likely to be diagnosed themselves
- ethnicity: there is a higher incidence of ulcerative colitis in Jewish populations; specifically those of Ashkenazi Jewish descent
- age: ulcerative colitis has a bimodal pattern of presentation; the predominant age of onset is between 15 and 30 years old, with a smaller, later onset between 50 and 70 years old
- gender: ulcerative colitis is more common in men than women, and men are more likely to experience later onset, with diagnosis in their 50s or 60s
- having an appendix: having an appendectomy decreases the risk of developing ulcerative colitis
- smoking history: ulcerative colitis occurs less frequently in current smokers; some evidence suggests smoking is a protective factor against the development of ulcerative colitis, but there is no confirmed link (CCFA, 2014; Lynch & Hsu, 2022)
Clinical Manifestations
The initial symptoms of ulcerative colitis are caused by inflammation of the rectum. These symptoms include bleeding, bowel movement urgency, and tenesmus (a feeling of rectal pressure that accompanies the need to have a bowel movement). Ulcerative colitis symptoms present intermittently, following a pattern of remission and exacerbation. The severity of intestinal damage influences symptoms. Changes leading to the loss of the absorptive mucosal surface and decreased transit time can result in large volumes of watery diarrhea. Destruction of the mucosal lining can lead to bleeding, abdominal cramping, and an increased urge to have a bowel movement. It is common for an individual to experience numerous episodes of bloody diarrhea accompanied by the passage of purulent mucus. When ulcerative colitis severity is mild, there is less mucosal involvement or involvement is limited to proctitis. Due to this decrease in intestinal damage, the prevalence of increased frequency of bowel movements, bleeding, and abdominal cramping are decreased. When the disease is severe, the entire colon can be affected. This can lead to additional symptoms, including fever, tachycardia, more than six bowel movements per day, urgency, bloody stools, severe continuous abdominal pain, dehydration, weight loss, and blood loss leading to anemia. Other complications that can occur with ulcerative colitis are systemic or affect specific areas outside the GI tract. These include cutaneous lesions, polyarthritis, sacroiliitis (inflammation of the sacroiliac joint), osteopenia and osteoporosis, oral ulcerations, episcleritis (inflammation of the episclera) or anterior uveitis of the eye (inflammation of the iris), sclerosing cholangitis of the liver, and increased incidence of cholelithiasis. The chronic inflammation that occurs with ulcerative colitis can also lead to changes in the coagulation pathway resulting in microthrombi or deep vein thrombosis (McCance & Huether, 2019).
There may be additional complications based on the areas affected, such as anal fissures, hemorrhoids, or a perirectal abscess. Although severe blood loss due to ulcerative colitis is rare, chronic blood loss can lead to hypotension and shock. The colon can sometimes become obstructed due to edema, strictures, or fibrosis. Although a rare complication, bowel perforation can occur (McCance & Huether, 2019). Table 1 outlines the most commonly experienced symptoms among patients with ulcerative colitis.
Table 1
Prevalence of Ulcerative Colitis Symptoms
Symptom | Experienced Ever | Experienced within 30 days |
Bowel movement urgency | 76% | 49% |
Abdominal pain or cramps | 73% | 47% |
Diarrhea (non-bloody) | 72% | 46% |
Tiredness, exhaustion, or fatigue | 71% | 48% |
Flatulence | 67% | 49% |
Bloating | 66% | 47% |
Bowel movement soon after eating | 64% | 37% |
Anxiety or depression | 53% | 32% |
Insomnia or sleeplessness | 49% | 30% |
Back pain | 47% | 31% |
(Elflein, 2021b)
Diagnostic Criteria
Any patient who presents with hematochezia (fresh, red blood in the stool) and bowel movement urgency should be suspected of having ulcerative colitis. An infectious cause of symptoms should be excluded, especially Clostridioides difficile (C. diff), Escherichia coli (E. coli), Salmonella, Shigella, Yersinia, Campylobacter, and parasitic infection (based on patient travel history or geographical location). A stool culture can eliminate an infectious cause of the patient's symptoms. Diagnosis of ulcerative colitis is based on the patient's medical history, clinical presentation, imaging, and biopsy results. When a colonoscopy is performed, the inflamed and hemorrhagic mucosa can be visualized. Radiology testing, using a computed tomography (CT) scan, can show the loss of the haustra (the pouches that give the colon a segmented appearance), the presence of ulceration, and irregular ulceration. Laboratory testing can also be performed to monitor hemoglobin, albumin, and potassium levels. Patients with ulcerative colitis have low hemoglobin, hypoalbuminemia, and hypokalemia. Other laboratory testing includes C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), which are both elevated with ulcerative colitis. Since the symptoms of ulcerative colitis overlap with Crohn's disease, the differential diagnosis can be challenging. A colonoscopy should be performed with intubation of the terminal ileum to confirm the diagnosis. Features seen upon endoscopic evaluation include a loss of vascular markings, erosion, and friability of the mucosa. When extensive inflammation is present, deep ulcerations and bleeding can be seen. Biopsies of affected and unaffected areas should be obtained and evaluated by a trained GI pathologist to confirm a diagnosis of ulcerative colitis. Biopsies of the unaffected areas are obtained since the disease may be present despite a normal presentation (McCance & Huether, 2019; Rubin et al., 2019).
Fecal calprotectin (FC) can be used as a noninvasive option to determine the extent of disease activity and response to therapy. FC is a neutrophil marker of inflammation that is often elevated in the presence of infectious or inflammatory colitis. However, FC is not elevated when the cause of symptoms is noninflammatory, such as irritable bowel syndrome (Rubin et al., 2019).
There are different categories of ulcerative colitis based on areas of involvement (Rubin et al., 2019). One standard used to classify the location of ulcerative colitis is the Montreal classification system. This classification system is outlined as follows:
- proctitis: affected areas are within 18 cm of the anal verge and distal to the rectosigmoid junction
- left-sided colitis: affected areas extend from the sigmoid colon to the splenic flexure
- extensive colitis: affected areas extend beyond the splenic flexure (Rubin et al., 2019)
There are also classification systems for the severity of ulcerative colitis. One of these classification systems is the Truelove and Witts system (Rubin et al., 2019). Initially published in 1955, this system outlines the severity of ulcerative colitis based on the following:
- mild colitis: less than four bowel movements per day, hemoglobin greater than 11 g/dL, ESR less than 20 mm/hr, and no changes to temperature or heart rate
- severe colitis: more than six bowel movements per day in the presence of fever, tachycardia, anemia, and elevated ESR (Rubin et al., 2019)
The Mayo endoscopic score is frequently used in clinical trials and practice to determine the severity of ulcerative colitis. A score of 0 equates to a normal finding or remission, whereas a score of 3 indicates severe active disease (Rubin et al., 2019). The Mayo endoscopic score is outlined in Table 2.
Table 2
Mayo Endoscopic Score
| Score |
| 0 | 1 | 2 | 3 |
Stool frequency | Baseline | 1-2 stools above baseline | 3-4 stools above baseline | 5 or more stools above baseline |
Rectal bleeding | Absent | Streaks of blood after wiping less than 50% of the time | Presence of blood most of the time | Presence of blood in the absence of stool |
Endoscopy results | Normal or signs of remission | The presence of slight erythema, mild friability, and decreased vascular pattern | The presence of erosions, friability, lack of vascular pattern, and erythema | The presence of ulcerations and unprompted bleeding |
Global assessment | Normal | Mild | Moderate | Severe |
(Rubin et al., 2019)
Recently, the ulcerative colitis endoscopic index of severity (UCEIS) was developed to score the disease severity based on endoscopy findings. Scoring is based on vascular pattern, the presence and extent of bleeding, and the appearance of erosions in the intestinal wall (Rubin et al., 2019). The UCEIS scoring is outlined in Table 3.
Table 3
Ulcerative Colitis Endoscopic Index of Severity (UCEIS)
| Score |
| 0 | 1 | 2 | 3 |
Vascular pattern | Normal | patchy obliteration; Decreased vascular pattern | Obliterated; Absence of vascular pattern | N/A |
Presence of blood | Absent | Mucosal; Areas of coagulated blood on the mucosal surface | Luminal mild; Presence of blood in the lumen | Luminal moderate or severe; Presence of frank blood in the lumen and visible oozing of blood from the mucosa following irrigation |
Erosions and ulcerations | Absent | Presence of erosions; Affected area ≤5 mm, white or yellow, with a flat edge | Superficial ulcer; Affected area > 5 mm and covered in fibrin | Deep ulcer; Affected area extends into the mucosa with the presence of a raised edge |
(Rubin et al., 2019)
Although this system is simple and easy to use, it does not provide a complete picture of clinical manifestations and the severity of endoscopic changes. Another classification system for the severity of ulcerative colitis is the American College of Gastroenterology Ulcerative Colitis Activity Index. This system is more robust and gives a more complete evaluation of disease severity since it incorporates laboratory values, endoscopic findings, and the results of the Mayo Endoscopic Scoring tool and the UCEIS (Rubin et al., 2019). This index is outlined in Table 4.
Table 4
American College of Gastroenterology Ulcerative Colitis Activity Index
| Remission | Mild | Moderate-Severe | Fulminant |
Stool frequency | Formed stools | < 4 per day | > 6 per day | > 10 per day |
Presence of hematochezia | Absent | Intermittent | Frequent | Continuous |
Bowel movement urgency | Absent | Occasional | Often | Always |
Hemoglobin | Baseline | Baseline | < 75% of baseline | < 7 g/dL |
ESR | < 30 mm/hr | < 30 mm/hr | > 30 mm/hr | > 30 mm/hr |
CRP | Normal | Increased | Increased | Increased |
FC | < 150-200 µg/g | > 150-200 µg/g | > 150-200 µg/g | > 150-200 µg/g |
Mayo endoscopic score | 0-1 | 1 | 2-3 | 3 |
UCEIS | 0-1 | 2-4 | 5-8 | 7-8 |
(Rubin et al., 2019)
Complications
Since ulcerative colitis is a chronic disease, complications can develop as the disease progresses. Common complications include a leak from anastomosis, the development of a pelvic abscess, enterocutaneous fistulas, fecal incontinence, sexual dysfunction, colon or rectal cancer, toxic megacolon, and pouch prolapse. The risk of colorectal cancer increases as the time since diagnosis increases. After 10 years, the risk is 2%, increasing to 8% after 20 years and 20% to 30% after 30 years. Over time, ulcerative colitis can lead to bowel perforation due to the weakened intestinal wall resulting from chronic inflammation. Severe inflammation can also lead to a rapid enlargement of the colon, known as toxic megacolon, a rare but deadly complication of ulcerative colitis (CCFA, 2014; Lynch & Hsu, 2022; Skomorochow & Pico, 2022).
Long-Term Management
Due to the changes that occur within the intestinal wall and complications of ulcerative colitis, individuals should undergo additional testing and monitoring. Due to the risk of colon cancer development in patients diagnosed with ulcerative colitis, a colonoscopy should be performed every 1 to 2 years. Individuals with a cervix should undergo annual cervical cancer screening. In addition, individuals should be screened regularly for signs and symptoms of depression and anxiety. Regular monitoring of bone density should also be performed due to the changes in absorption that can occur due to intestinal wall changes. As a result of immune changes and the effects of treatment with biological agents, individuals should be vaccinated against herpes zoster, pneumococcus, H. influenza, and influenza. Individuals should also not travel to areas with a high risk of contracting yellow fever. Individuals should also be screened at least yearly for signs of skin malignancies due to treatment with biological agents (Lynch & Hsu, 2022).
Surgical Management
Since ulcerative colitis is typically restricted to the colon, a colectomy is considered a curative treatment. A colectomy is indicated in patients who have not achieved remission despite medication management or experience intolerable adverse effects due to medication management. Surgical intervention is also indicated for patients with toxic megacolon, bowel perforation, bleeding, strictures, intractable fulminant colitis, or cancer. The standard surgical treatment is a restorative proctocolectomy with ileal pouch-anal anastomosis (RPC-IPAA). An RPC-IPAA is a 2-step procedure. During the first step, the colon and most of the rectum are removed, leaving the anus and anal sphincter untouched. Then, a surgical pouch is created using the last 1.5 feet of the small intestine. A temporary loop ileostomy is created to allow the surgically created pouch to heal. The second stage involves reversing the temporary loop ileostomy. This can occur in as little as 1 to 2 months after stage 1. Some patients may not be good candidates for an RPC-IPAA. In these cases, a total proctocolectomy with permanent ileostomy is indicated. During this procedure, the colon, rectum, and anus are removed, and the anus is surgically closed. The end of the ileum is then diverted through the abdominal wall, creating a stoma (Ignatavicius et al., 2018; Lynch & Hsu, 2022).
Crohn's Disease
Crohn's disease is a type of IBD that affects the GI tract at any point from the mouth to the anus; however, it most commonly affects the distal portion of the small intestine and the proximal portion of the large intestine. It is an idiopathic disorder of unknown etiology. Crohn's disease develops slowly and progresses unpredictably. The disease affects multiple areas of the intestine, with the presence of normal, unaffected regions in between. This disease pattern is known as skip lesions and appears as a cobblestone pattern. The symptoms of Crohn's disease occur in a waxing and waning pattern with periods of active disease and remission (Ignatavicius et al., 2018).
Epidemiology
Approximately 1 million individuals are living with Crohn's disease in the US. Globally, Canada has the highest incidence of Crohn's disease. Of those with Crohn's disease, 35% have involvement of the ileum only (ileitis), 45% have involvement of the ileum and colon (ileocolitis), with more involvement on the right side of the colon, and 20% have involvement of the colon only (granulomatous colitis) without the involvement of the rectum (Walfish & Companioni, 2022a).
Pathophysiology
Crohn's disease begins with inflammatory lesions in the intestinal submucosa and spreads sporadically, which, as discussed above, is known as skip lesions. The progression of Crohn's disease is unpredictable, and one side of the small intestine may be affected while the other may not. Progression involves neutrophils infiltrating the crypts, resulting in the development of abscesses and the destruction of the crypts. Ulcerations caused by Crohn's disease appear as longitudinal and transverse fissures that can extend into the lymphoid tissue. The typical presentation of Crohn's disease lesions is a granuloma surrounded by areas of ulceration (McCance & Huether, 2019).
Risk Factors
There are many modifiable and nonmodifiable risk factors associated with Crohn's disease. Some risk factors overlap with those seen with ulcerative colitis, while others are distinct. Risk factors for the development of Crohn's disease include:
- family history
- smoking history
- ethnicity: Crohn's disease is more common in those with an Ashkenazi Jewish background
- geographical location: those living in urban areas are more at risk of developing Crohn's disease
- gender: women are affected slightly more than men
- age: onset usually occurs before the age of 40
- history of an appendectomy: having the appendix surgically removed increases an individual's risk of developing Crohn's disease
- gene mutation: there is a strong association between Crohn's disease and alterations in the nucleotide-binding-oligomerization-domain-containing protein 2 (CARD15/NOD2) gene found on chromosome 16 (CCFA, 2014; McCance & Huether, 2019)
Clinical Manifestations
Typically, in the early stages of Crohn's disease, individuals have no other symptoms besides reports of an irritable bowel. Symptoms associated with Crohn's disease can be localized to the GI tract or systemic. The symptoms are similar to those seen with ulcerative colitis but can vary depending on the area of the affected intestine and the disease's extent. The most common symptom of Crohn's disease is chronic diarrhea. Other GI symptoms include abdominal pain, unintentional weight loss, and anal pain. Anal pain can be attributed to anal fissures, ulcers, fistulas, or stenosis. Additional symptoms and complications may include fatigue, aphthous stomatitis (oral ulcerations), joint pain, osteonecrosis, cholelithiasis, and uveitis or scleritis. A diagnosis of Crohn's disease can also be associated with other immune-mediated disorders, including asthma, pericarditis, psoriasis, celiac disease, multiple sclerosis, rheumatoid arthritis, and chronic bronchitis (Lichtenstein et al., 2018; McCance & Huether, 2019). Symptoms of Crohn's disease are patient-dependent. Table 5 lists the most commonly experienced symptoms. The presence of symptoms is broken down into those experienced at any point during the disease compared with those experienced in the last 30 days (Elflein, 2021).
Table 5
Prevalence of Crohn's Disease Symptoms
Symptom | Experienced Ever | Experienced within 30 days |
Diarrhea (non-bloody) | 79% | 58% |
Abdominal pain or cramps | 77% | 53% |
Bowel movement urgency | 75% | 52% |
Tiredness, exhaustion, or fatigue | 73% | 56% |
Nausea and vomiting | 71% | 39% |
Bloating | 70% | 52% |
Bowel movement soon after eating | 69% | 46% |
Flatulence | 69% | 52% |
High stool frequency | 62% | 37% |
Anxiety or depression | 58% | 37% |
(Elflein, 2021a)
Diagnostic Criteria
The diagnosis of Crohn's disease is similar to ulcerative colitis. It is based on clinical presentation and endoscopic, pathologic, and histologic results. Laboratory testing may also be performed to assess for inflammation, anemia, dehydration, and malnutrition. Laboratory results typically show a decrease in hemoglobin and an increase in platelets. CRP is elevated due to the inflammation that occurs with Crohn's disease. ESR may also be elevated due to inflammation; however, it will not differentiate between Crohn's disease and another disorder that causes inflammation. Approximately 40% of patients with Crohn's disease will have a normal CRP and ESR (Lichtenstein et al., 2018).
Endoscopic testing can be completed via a colonoscopy or through the use of an ingestible camera. Abdominal X-rays may also be performed and can show a narrowing of the intestine and the presence of ulcerations, strictures, and fistulas. Magnetic resonance enterography (MRE) can also assess bowel motility. An abdominal ultrasound or CT scan may demonstrate the extent of the disease. An FC test should be performed to differentiate between IBD and IBS, and the patient should be tested for an infectious cause of symptoms (Ignatavicius et al., 2018).
Endoscopic scoring systems have been developed to quantify the changes in the intestinal mucosa due to Crohn's disease. Examples of these scoring systems include the Endoscopic Index of Severity (CDEIS) and the Simple Endoscopic Score for Crohn's disease (SES-CD). The CDEIS uses a point system to determine the severity of the disease. Areas assessed include the rectum, sigmoid or left colon, transverse colon, right colon, and ileum. If deep ulcerations are present, a score of 12 is assigned for each location where the ulcers are present. The presence of superficial ulcerations equates to a score of 6 for each site. Surface involvement of the disease and ulcerations is scored based on the length of involvement in centimeters. All results are added and divided by the number of segments that could be visualized either partially or entirely. If ulcerated or non-ulcerated stenosis is present in any of the segments, 3 points for each finding are added to the total to generate the final CDEIS score. A score of less than 3 equates to remission, a score of 3 to 8 indicates mild endoscopic activity, a score of 9-12 indicates moderate endoscopic activity, and a score greater than 12 indicates severe endoscopic activity present. The SES-CD is the most widely used due to its ease of use (Lichtenstein et al., 2018). The SES-CD is described in Table 6.
Table 6
Simple Endoscopic Score for Crohn's Disease
| 0 | 1 | 2 | 3 |
Size of ulcers | Absent | Aphthous ulcers (0.1 cm to 0.5 cm) | Large ulcers (0.5 cm to 2.0 cm) | Very large ulcers (> 2.0 cm) |
Ulcerated surface | Absent | < 10% | 10% to 30% | > 30% |
Affected surface | Unaffected | < 50% | 50% to 70% | > 75% |
Narrowing | Absent | Single; stool can pass | Multiple; stool can pass | Stool unable to pass |
(Lichtenstein et al., 2018)
Complications
Complications related to a diagnosis of Crohn's disease are similar to those associated with ulcerative colitis. While hemorrhage is possible with Crohn's disease, it is less common. The most common complication is malabsorption due to changes in the small intestine. Cancer of the colon or small intestine is rarer in Crohn's disease but may occur after the disease has been present for at least 15 to 20 years. Fistula development is more likely with Crohn's disease than ulcerative colitis. A fistula can develop between segments of the intestine, as a perirectal abscess, opening in the skin, or as an extension to another organ structure (e.g., the vagina or bladder). The thickened lining that results from chronic inflammation can lead to the development of strictures that can cause a bowel obstruction (Ignatavicius et al., 2018). Other complications of Crohn's disease may include:
- ankylosing spondylitis
- episcleritis or iritis
- cholelithiasis
- anemia; due to vitamin B12 deficiency because of malabsorption
- hypercoagulable state
- osteoporosis; due to deficiencies in vitamin D and calcium due to malabsorption
- renal calculi
- erythema nodosum (a condition characterized by red bumps on the shins)
- pyoderma gangrenosum (a condition that results in large, painful leg ulcers; Ranasinghe & Hsu, 2022)
Treatment of Inflammatory Bowel Disease
Treatment options are based on disease severity and patient presentation. Guidelines for treatment consider patient-reported outcomes, including normalizing bowel habits or decreased bleeding. Treatment guidelines also change based on the inflammatory burden, extent and severity of inflammation, disease course, whether hospitalization or steroids are indicated, if there is a failure in conservative treatment options, and disease impact on the patient's quality of life. Treatment should also be guided by the specific diagnosis, disease severity, and prognosis (Rubin et al., 2019; Walfish & Companioni, 2022b).
First-line treatment for ulcerative colitis is a class of medications known as aminosalicylates (5-ASAs). These drugs are also used for maintenance therapy. Although 5-ASAs are used to treat mild to moderate Crohn's disease, they are not approved by the US Food and Drug Administration (FDA) for this indication. Some guidelines recommend utilizing antibiotics as first-line treatment, whereas others suggest delaying antibiotic initiation until the completion of 4 weeks of treatment with a 5-ASA with no improvement. However, other guidelines consider corticosteroids the first-line treatment of Crohn's disease, with 5-ASA drugs reserved for those who do not see improvement in symptoms or cannot tolerate corticosteroid use (CCFA, 2022; Rubin et al., 2019; Walfish & Companioni, 2022a, 2022b).
The 5-ASA class of drugs includes sulfasalazine (Azulfidine), mesalamine (Asacol HD, Pentasa, Lialda, Apriso, Delzicol), olsalazine (Dipentum), and balsalazide (Colazal). These drugs work by decreasing inflammation in the GI tract. They are most effective in the colon and can be administered rectally via an enema or suppository or orally as an extended-release formulation (CCFA, 2022; Rubin et al., 2019; Walfish & Companioni, 2022b). Dosing of the 5-ASA medications is as follows:
- sulfasalazine (Azulfidine) initial dose 0.5 g orally two times daily, increasing the dose over several days to 1 - 1.5 g orally four times daily based on patient presentation and tolerance to treatment
- olsalazine (Dipentum) 1000 mg orally two times daily
- balsalazide (Colozal) 2.25 grams orally three times daily
- mesalamine is available as a delayed-release or extended-release formulation under many brand names, each with specific dosing
- Asacol HD 1600 mg orally three times daily
- Pentasa 1 g orally four times daily
- Lialda 2,400 mg to 4,800 mg orally once daily
- Apriso 1500 mg orally once daily
- Delzicol 800 mg orally three times daily (Walfish & Companioni, 2022b)
For patients with proctitis or left-sided colon involvement, 5-ASA therapy can be given rectally as a suppository at 500 mg to 1,000 mg at bedtime or in divided doses twice daily. This medication can also be administered rectally as an enema at a dose of 4 grams at bedtime or in divided doses twice daily. Rectal formulations can be used in addition to oral therapy as acute or maintenance treatment (Rubin et al., 2019; Walfish & Companioni, 2022b).
Due to the presence of sulfa, sulfasalazine (Azulfidine) has the most adverse effects. These include nausea, dyspepsia, fever, rash, nervousness, sensitivity to sunlight, and headache. Taking the medication with food can decrease some of these effects. Sulfa can also disrupt folate absorption (folic acid) and cause hemolytic anemia, agranulocytosis, hepatitis, pneumonitis, or myocarditis. Sulfasalazine (Azulfidine) can also cause decreased sperm count and motility; this adverse effect has been reported in 80% of men but is reversible following treatment discontinuation. Due to the disruption of folate (folic acid) absorption, individuals should take 1 mg of folate daily. Individuals taking sulfasalazine (Azulfidine) should also undergo laboratory testing, including complete blood count (CBC) and liver function tests every 6 to 12 months. Sulfasalazine (Azulfidine) is contraindicated in individuals with an allergy to sulfa as there is a cross-reaction. If mild allergic reaction symptoms present but the medication is effective in managing IBD symptoms, a desensitization regimen, starting with a very low dose and slowly increasing based on patient tolerance, can be introduced to minimize adverse effects. Side effects of the other 5-ASA medications include malaise, headache, hair loss, colitis, and pancreatitis. Olsalazine (Dipentum) can cause watery diarrhea in approximately 15% of individuals and occurs more frequently in those with pancolitis (Chiefetz & Cullen, 2022; Walfish & Companioni, 2022b).
Individuals diagnosed with Crohn's disease may need to be treated with antibiotics to treat the presence of bacterial infection in the GI tract. Infections associated with Crohn's disease may include abscesses and fistulas involving the anal canal and vagina. Examples of antibiotics commonly prescribed to treat infections in patients with Crohn's disease include metronidazole (Flagyl), ciprofloxacin (Cipro), and rifaximin (Xifaxan; CCFA, 2022). Dosing of the antibiotics used for Crohn's disease are as follows:
- metronidazole (Flagyl) 500 mg to 750 mg orally three times daily for 4 to 8 weeks
- ciprofloxacin (Cipro) 500 mg to 750 mg orally two times daily; some guidelines recommend utilizing ciprofloxacin (Cipro) in combination with metronidazole (Flagyl)
- rifaximin (Xifaxan) 200 mg orally three times daily or 800 mg orally two times daily (Walfish & Companioni, 2022b)
When patients do not experience remission following treatment with a 5-ASA medication, switching to an alternative 5-ASA medication is not recommended. Instead, a corticosteroid should be added to the treatment regimen. Corticosteroids are also indicated in moderate to severe Crohn's disease. Examples of corticosteroids used in the treatment of ulcerative colitis are prednisone (Deltasone), hydrocortisone (Cortef), methylprednisolone (Medrol), and budesonide (Entocort, Uceris; CCFA, 2022; Rubin et al., 2019). Dosing of the corticosteroids used in IBD treatment are as follows:
- prednisone (Deltasone) is the 1st line treatment recommended; the initial dose is 40 mg to 60 mg daily as a single dose
- hydrocortisone (Cortef) can be administered as an enema to treat proctitis or left-sided colon involvement; dosing is 100 mg in 60 mL of an isotonic solution 1 to 2 times daily; if effective, treatment should be continued every day for 2 to 4 weeks and then titrated down to every other day for 1 to 2 weeks, then gradually spaced out until discontinuation after an additional 1 to 2 weeks; for severe disease in an acute care setting, it can be administered intravenously at a dose of 300 mg per day
- methylprednisolone (Medrol) is used in severe disease; initial dosing is 16 mg to 20 mg administered intravenously three times daily
- budesonide (Entocort, Uceris) 9 mg orally once daily (Walfish & Companioni, 2022b)
Symptoms should begin improving after 5 to 7 days of treatment. The duration of treatment should be as short as possible to reach the remission of symptoms, usually 7 to 28 days, followed by tapered discontinuation due to the adverse effects associated with long-term corticosteroid use and abrupt cessation of treatment. Adverse effects include edema, gastritis, hypertension, fluid and electrolyte imbalances, immunosuppression, increased appetite, weight gain, insomnia, psychosis, hyperglycemia, and cushingoid symptoms. Corticosteroids must be used cautiously in patients with renal disease, hypertension, osteoporosis, seizures, heart failure, psychosis, and emotional instability (CCFA, 2022; Rubin et al., 2019; Woods, 2023).
If remission is not achieved after adding a corticosteroid, a thiopurine or biological drug can be added to the treatment regimen. Thiopurines are immunosuppressants. These drugs suppress the body's immune response to prevent and reduce inflammation. Examples of thiopurines include azathioprine (Imuran) and 6-mercaptopurine (Purinethol). Azathioprine (Imuran) and its metabolite 6-mercaptopurine (Purinethol) can inhibit T-cell function as part of the immune response and may even induce T-cell apoptosis. These medications can be effective in the long-term management of IBD and may decrease the need for corticosteroids. These drugs can help maintain remission for multiple years and achieve clinical benefits in as little as 1 to 3 months (CCFA, 2022; Lynch & Hsu, 2022; Walfish & Companioni, 2022b). The dosing of these medications is as follows:
- azathioprine (Imuran) 2.5 mg/kg to 3.0 mg/kg orally once daily
- 6-mercaptopurine (Purinethol) 1mg/kg to 1.5 mg/kg orally once daily (Walfish & Companioni, 2022b)
The most common adverse effects of these medications are nausea, vomiting, and malaise. Other adverse effects include pancreatitis and hepatotoxicity. Due to the suppression of T-cells, these medications are associated with an increased risk of lymphoma and nonmelanoma skin cancers. White blood cell counts should be assessed biweekly for 1 month after initiation of treatment and then every 1 to 2 months to monitor for signs of bone marrow suppression. Liver function studies should be performed every 6 to 12 months to monitor for signs of hepatotoxicity (Walfish & Companioni, 2022b).
Patients diagnosed with Crohn's disease who require corticosteroids to manage symptoms or have not had symptoms adequately managed despite corticosteroid use and have not responded to the initiation of azathioprine (Imuran) or 6-mercaptopurine (Purinethol) can benefit from treatment with methotrexate (Trexall). Dosing is 15 mg to 25 mg administered orally or subcutaneously once weekly. Side effects include nausea, vomiting, neurotoxicity, fatigue, dizziness, aphasia, fever, blurred vision, diarrhea, cirrhosis, arthralgia, rash, photosensitivity, and alopecia. Those individuals of reproductive age, and their partners, should utilize an effective form of birth control such as an intrauterine device, implant, or oral contraceptive. Before attempting to conceive, methotrexate (Trexall) should be discontinued for at least 3 months. CBC, liver function tests, and albumin should be monitored monthly for the first 3 months of therapy, then every 8 to 12 weeks. If 6 of the 12 liver function tests performed in a year show an elevated aspartate aminotransferase (AST), a liver biopsy should be performed to assess for liver damage. Methotrexate (Trexall) is contraindicated in patients with hepatitis B, hepatitis C, diabetes, obesity, and current alcohol abuse (Walfish & Companioni, 2022b).
Biological drugs are antibodies that inhibit proteins from causing inflammation, specifically tumor necrosis factor (TNF). Examples of biological drugs include infliximab (Remicade), adalimumab (Humira), certolizumab (Cimzia), and golimumab (Simponi). Infliximab (Remicade), adalimumab (Humira), and certolizumab (Cimzia). These drugs can be used in Crohn's disease to prevent recurrence following remission. Infliximab (Remicade), adalimumab (Humira), and golimumab (Simponi) can be used in patients with refractory or corticosteroid-dependent ulcerative colitis. Of the biological drugs, infliximab (Remicade) is the most commonly used to treat ulcerative colitis (CCFA, 2022; Lynch & Hsu, 2022; Walfish & Companioni, 2022b). The dosing of these medications is as follows:
- infliximab (Remicade) 5 mg/kg administered intravenously over 2 hours; dosing is repeated at 2 weeks, 6 weeks, and then every 8 weeks; to maintain remission after a year, the dosage must be increased, or the duration between dosing decreased; serum drug levels should be monitored to maintain a therapeutic level > 5 mcg/mL; individuals that do not respond to infliximab (Remicade) or begin to experience treatment failure over time may benefit from a change to adalimumab (Humira)
- adalimumab (Humira) initial loading dose of 160 mg administered subcutaneously, then 80 mg at week 2, then 40 mg administered every 2 weeks; dosing should be adjusted to maintain a therapeutic serum level of > 7.5 mcg/mL
- certolizumab (Cimzia) 400 mg administered subcutaneously every 2 weeks for three doses, then every 4 weeks; dosing should be adjusted to maintain a serum level > 20 mcg/mL
- golimumab (Simponi) initial loading dose of 200 mg administered subcutaneously with a follow-up dose of 100 mg given at week 2, then 100 mg given every 4 weeks (Walfish & Companioni, 2022b)
These medications can be used as monotherapy or with a thiopurine or methotrexate (Trexall). Adverse effects can include fever, chills, headache, nausea, and immediate or delayed hypersensitivity reactions presenting as a rash, pruritis, or anaphylactic reaction. Sepsis can occur following treatment with anti-TNF medications; therefore, these medications are contraindicated in patients with an active infection. It is also important to test patients for latent tuberculosis or hepatitis B, as these diseases can be reactivated by treatment with anti-TNF medications (Walfish & Companioni, 2022b).
Another treatment option includes vedolizumab (Entyvio) and natalizumab (Tysabri); both belong to a novel class of biological drugs that function as antibodies to leukocyte adhesion molecules and are therefore known as anti-adhesion molecule inhibitors. These drugs are FDA-approved to treat moderate to severe ulcerative colitis and Crohn's disease. Vedolizumab (Entyvio) initial dosing is 300 mg administered intravenously, followed by repeat dosing at weeks 2 and 6, then every 8 weeks. Although administered intravenously, the effects of vedolizumab (Entyvio) are limited to the GI tract. If there is no improvement in patient symptoms after 14 weeks of treatment, the medication should be discontinued. Adverse effects include fatigue, headaches, arthralgia, cough, fever, sinusitis, and infection. Due to its higher incidence of systemic effects, natalizumab (Tysabri) is reserved for second-line treatment, following vedolizumab (Entyvio). Dosing is 300 mg administered intravenously over 1 hour every 4 weeks. Due to adverse effects, natalizumab (Tysabri) authorization is required as it is only available through a restricted prescribing program, and treatment should be reassessed every 6 months. Adverse effects include headaches, fatigue, arthralgia, depression, and the development of progressive multifocal leukoencephalopathy (PML). Therefore, vedolizumab (Entyvio) is contraindicated in any individual with a history of PML (Walfish & Companioni, 2022b).
Ustekinumab (Stelara) is an anti-IL-12/23 antibody approved for use in individuals with moderate to severe ulcerative colitis or Crohn's disease that have failed treatment with conventional therapy. Ustekinumab (Stelara) is initially administered intravenously following weight-based dosing. For individuals less than 55 kg, the initial dose is 260 mg; for those between 55 kg and 85 kg, the initial dose is 390 mg; and for those above 85 kg, the initial dose is 520 mg. After the initial loading dose, the maintenance dose is 90 mg, administered subcutaneously every 8 weeks. Adverse effects include depression, dizziness, fatigue, headaches, fever, diarrhea, nausea, vomiting, abdominal pain, and increased risk for infection. Ustekinumab (Stelara) is contraindicated in individuals with an active infection (Walfish & Companioni, 2022b; Woods, 2023).
Individuals with moderate to severe ulcerative colitis can be treated with target synthetic small-molecule medications. These drugs have a molecular weight of less than 1 kilodalton, and they differ from monoclonal antibodies as they lack the same immunogenicity and can be administered orally. These drugs reduce inflammation by directly targeting specific steps in the immune response. Examples include tofacitinib (Xeljanz) and ozanimod (Zeposia; CCFA, 2022; Walfish & Companioni, 2022b).
Tofacitinib (Xaljanz) specifically inhibits Janus kinas 1-3. It is available in immediate-release and extended-release formulations. Immediate-release initial dosing is 10 mg orally two times daily for 8 weeks, then 5 mg to 10 mg orally two times daily. Extended-release initial dosing is 22 mg orally once daily for 8 weeks, then 11 mg orally once daily. Adverse effects include hypercholesterolemia, diarrhea, headaches, rash, upper respiratory infection, and reactivation of herpes zoster in the form of shingles. There is a black box warning of the increased risk of pulmonary embolism and death in individuals with rheumatoid arthritis (CCFA, 2022; Walfish & Companioni, 2022b).
Ozanimod (Zeposia) is a sphingosine 1-phosphate (S1p) receptor modulator. Initial dosing is 0.23 mg administered orally on days 1-4, then 0.46 mg on days 5-7, then 0.92 mg daily beginning on day 8. If any dose is missed within the first 14 days of treatment, the titration should be restarted at 0.23 mg. Adverse effects include rash, urticaria, bradycardia, hypertension, orthostatic hypotension, atrioventricular (AV) block, dyspnea, and increased risk of infection. Due to the cardiac effects of ozanimod (Zeposia), it is contraindicated in individuals with a history of myocardial infarction within the last 6 months, unstable angina, and heart failure. It is also contraindicated in patients with conduction disorders unless they have a functioning pacemaker implanted (CCFA, 2022; Walfish & Companioni, 2022b).
Patient Education
The goals of IBD management include pain control and proper skin care. To decrease abdominal pain, the patient should administer analgesics as ordered and report changes in the effectiveness of the treatment regimen. The patient should keep a log or diary of all fluid and food intake to help determine if certain foods exacerbate symptoms. Although there is no direct relationship between diet and IBD, many patients report exacerbations following the ingestion of caffeine, alcohol, raw vegetables, foods high in fiber, and those containing lactose or gluten. It is also important that patients monitor their weight. Patients should be counseled on proper skin care to prevent breakdown, including washing the perineal area with mild soap and water after each bowel movement and patting the area dry. If irritation occurs, sitz baths followed by a thin application of A & D ointment may be beneficial. Patients should be encouraged to report changes in their elimination pattern, including altered frequency, amount, presence of blood, and consistency of bowel movements. Patients should be educated on the importance of follow-up care, the availability of community resources, and signs and symptoms to report to the HCP (Ignatavicius et al., 2018).
References
Cheifetz, A. S., & Cullen, G. J. (2022). Patient education: Sulfasalazine and the 5-aminosalicylates (Beyond the basics). UpToDate. Retrieved December 22, 2022, from https://www.uptodate.com/contents/sulfasalazine-and-the-5-aminosalicylates-beyond-the-basics
Crohn's and Colitis Foundation of America. (2014). The facts about inflammatory bowel diseases. https://www.crohnscolitisfoundation.org/sites/default/files/2019-02/Updated%20IBD%20Factbook.pdf
Crohn's and Colitis Foundation of America. (2022). Understanding IBD medications and side effects. https://www.crohnscolitisfoundation.org/sites/default/files/2022-09/understanding-ibd-medications-brochure-final-rev0822-3_1.pdf
Elflein, J. (2021a). Most common Crohn's disease symptoms among Crohn's patients worldwide as of 2019. https://www.statista.com/statistics/1208470/most-common-symptoms-for-crohns-disease-patients-worldwide
Elflein, J. (2021b). Most common symptoms among ulcerative colitis patients worldwide in 2019. https://www.statista.com/statistics/1208499/most-common-symptoms-ulcerative-colitis-among-worldwide-patients
Goran tek-en. (2014). Layers of the GI tract [Image]. https://commons.wikimedia.org/wiki/File:Layers_of_the_GI_Tract_english.svg
Ignatavicius, D. D., Workman, M. L., & Rebar, C. R. (2018). Medical-surgical nursing: Concepts for interprofessional collaborative care (9th ed.). Elsevier.
Lichtenstein, G. R., Loftus, E. V., Isaacs, K. L., Regueiro, M. D., Gerson, L. B., & Sands, B. E. (2018). ACG clinical guideline: Management of Crohn's disease in adults. American Journal of Gastroenterology, 113(4), 481-517. https://doi.org/10.1038/ajg.2018.27
Lynch, W. D., & Hsu, R. (2022). Ulcerative colitis. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK459282
McCance, K. L., & Huether, S. E. (2019). Pathophysiology: The biologic basis for disease in adults and children (8th ed.). Elsevier.
McDowell, C., Farooq, U., & Haseeb, M. (2022). Inflammatory bowel disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470312
Ranasinghe, I. R., & Hsu, R. (2022). Crohn disease. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK436021
Rubin, D. T., Ananthakrishnan, A. N., Siegel, C. A., Sauer, B. G., & Long, M. D. (2019). ACG clinical guideline: Ulcerative colitis in adults. The American Journal of Gastroenterology, 114(3), 384-413. https://doi.org/10.14309/ajg.0000000000000152
Skomorochow, E., & Pico, J. (2022). Toxic megacolon. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK547679
Terlizzi, E. P., Dahlhamer, J. M., Xu, F., Wheaton, A., Greenlund, K. J., & National Center for Chronic Disease Prevention and Health Promotion. (2021). Health care utilization among U.S. adults with inflammatory bowel disease, 2015-2016. National Health Statistics Reports, 152. https://doi.org/10.15620/cdc:100471
Walfish, A. E., & Companioni, R. A. C. (2022a). Crohn disease. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gastrointestinal-disorders/inflammatory-bowel-disease-ibd/crohn-disease
Walfish, A. E., & Companioni, R. A. C. (2022b). Drugs for inflammatory bowel disease. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gastrointestinal-disorders/inflammatory-bowel-disease-ibd/drugs-for-inflammatory-bowel-disease
WolfpackBME. (2022). Inflammatory bowel disease [Image]. https://commons.wikimedia.org/wiki/File:Inflammatory_Bowel_Disease_MTK.jpg
Woods, A. D. (2023). Nursing2023 drug handbook (43rd ed.). Wolters Kluwer.
Xu, F., Dahlhamer, J. M., Zammitti, E. P., Wheaton, A. G., & Croft, J. B. (2018). Health-risk behaviors and chronic conditions among adults with inflammatory bowel disease - United States, 2015 and 2016. Morbidity and Mortality Weekly Report (MMWR), 67(6), 190-195. https://doi.org/10.15585/mmwr.mm6706a4
Powered by Froala Editor