About this course:
This learning module reviews relevant terminology and explores the current research on best practices related to wound care.
Course preview
Interdisciplinary Wound Care
This learning module reviews relevant terminology and explores the current research on best practices related to wound care.
After this activity, learners will be prepared to:
- recognize the normal anatomy and physiology of the skin
- differentiate between types of acute and chronic wounds
- describe factors that impact the normal healing processes
- explain the nurse's role in assessing and documenting wounds
- identify interventions the nurse uses to prevent acute and chronic wounds
- explore treatment options for different categories of wounds and interdisciplinary collaboration
Anatomy and Physiology of the Skin
The skin is the largest human organ, accounting for approximately 20% of the total body weight. The skin's primary function is to protect internal organs and structures from biological invasion, ultraviolet radiation, fluid loss, and physical damage. Additional functions of the skin are thermoregulation through sweating and regulation of blood flow, synthesis of Vitamin D, the sensation from nerve endings, excretion of salts and small amounts of waste products, and provision of aesthetics and communication. The skin comprises the epidermis (outer layer), the dermis (middle layer), and the hypodermis (the deepest or subcutaneous layer; refer to Figure 1). The health of the skin influences overall health and has a profound psychological significance because it identifies each individual with unique facial and body characteristics. Self-image may be enhanced or deterred by society's standards for appearance (Rogers & Brashers, 2023).
Figure 1
Structure of the Skin
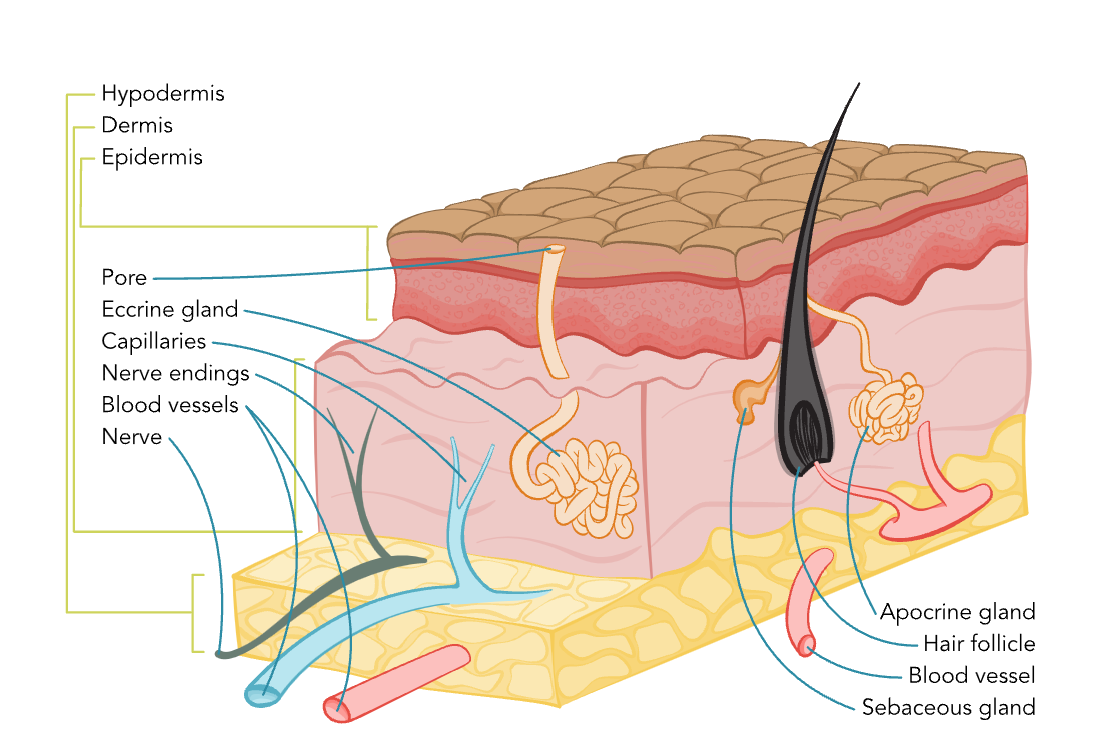
The epidermis acts as a defensive barrier that is constantly renewed by shedding the superficial layer (stratum corneum). The epidermis is composed primarily of keratinocytes embedded in a lipid matrix. The epidermis is slightly acidic, with a pH of 4.5 to 6 and comprises five layers, including the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. Each layer has a function and plays a role in the healing process of wounds (Rogers & Brashers, 2023).
The stratum corneum is composed of tough superficial sheets of cornified cells. This layer is also waterproof. Forming the outermost layer, it consists of fibrous dead cells that help to regulate pH and temperature and provide protection. It is very thin, measuring only 0.05 mm on the eyelids and 1.5 mm on the soles of the feet and palms of the hands; however, it can thicken with frequent pressure or friction (e.g., calluses or corns). This layer is continuously being replaced and helps with the skin's ability to repair itself.
The stratum lucidum consists of layers of cells containing eleidin, which become keratin as cells move up to the stratum corneum layer. The stratum lucidum is only found in palmoplantar skin to provide extra protection because these areas are exposed to more significant deterioration.
The stratum granulosum is the layer where keratinocytes lose their nuclei, flatten, and die. Keratinization (i.e., the increased production of the protein keratin) occurs in this layer and helps reduce water loss from the epidermis. The stratum spinosum is 8 to 10 cells thick and contains cells with spiny processes called desmosomes. This layer also contains Langerhans cells (a type of dendritic cell), which can initiate an immune response.
The stratum basale (basal layer) is also known as the basement membrane and forms the lowest layer of the epidermis. This layer is one cell thick and forms a border between the epidermis and dermis. It constantly makes new keratinocytes that flatten as they move up to the surface, replacing cells that have been shed from the stratum corneum. This process takes between 28 and 35 days. Cells continuously divide for the ongoing rejuvenation of the skin. Melanocytes are also produced in the stratum basale (Rogers & Brashers, 2023).
The dermis is the layer below the epidermis. It is 1 to 4 mm thick and composed of three types of connective tissue (collagen, elastin, reticulin) and a gel-like ground substance. The primary role of the dermis is to support and provide nutrition to the epidermis. This layer consists primarily of collagen, a tough, fibrous protein that helps skin resist tearing. The dermis is resilient and elastic, allowing the skin to stretch with body movement. The dermis houses the nerves, sensory receptors, blood vessels, lymphatics, hair follicles, sebaceous glands, and sweat glands (Rogers & Brashers, 2023).
The third layer of skin is the hypodermis or subcutaneous tissue. This layer connects the dermis to the underlying muscle. It comprises blood vessels, adipose tissue, and connective tissue that support the dermis. Macrophages, fibroblasts, nerves, and hair follicle roots are also found within this layer. The fat stored in this layer provides internal structures with additional protection and insulation against cold temperatures (Rogers & Brashers, 2023).
Types of Wounds
Wounds are either acute or chronic. Acute wounds often have an identifiable cause that leads to skin integrity loss and usually results from trauma. Acute wounds are present in various depths, sizes, and anatomical locations. Acute wounds can also be created in a controlled surgical environment. Chronic wounds can develop over time from an acute traumatic injury or surgical wound. Chronic wounds often affect individuals with a physiologic process that delays or prevents proper wound healing, such as diabetes, peripheral vascular disease (PVD), immunodeficiency, and malnutrition. Currently, no clearly defined period indicates an acute wound has become a chronic wound; however, some guidelines suggest that an acute wound becomes chronic after six weeks or in the absence of a weekly 15% reduction in wound surface area or a 50% reduction in a month (Armstrong & Meyr, 2024a; Nagle et al., 2023).
There are many different mechanisms of wounds (Armstrong & Meyr, 2024a; Nagle et al., 2023; Singer, 2022).
- Abrasions and scrapes occur when a mechanical force, such as friction against a hard surface, scrapes away a partial-thickness area of the skin. These wounds vary in size and depth and can be complicated by dirt or debris embedded in the wound bed (Shrestha et al., 2023; Singer, 2022).
- Bites can originate from animals or humans, but the impact can be equally severe. A dog, cat, or rodent bite can introduce infectious diseases, including rabies, into the wound. Injury to the tissue can occur secondary to the teeth and the force of the bite and movement of the animal as their teeth clamp down onto the tissue. A human bite can introduce bacteria from the mouth, including Staphylococcus aureus, streptococci, syphilis, tuberculosis, or viruses such as hepatitis B (HBV), hepatitis C, and herpes simplex virus. Although not commonly reported, a human bite can transmit the human immunodeficiency virus (HIV). Any bite can lead to severe complications such as osteomyelitis or infectious arthritis (Baddour & Harper, 2024; Barrett, 2024).
- Burns can be caused by thermal extremes, electricity, caustic chemicals, or radiation. The extent of damage from burns is dependent on the source, duration of contact or exposure, and anatomical location of the injury. Preexisting conditions (e.g., diabetes, peripheral vascular disease (PVD), immunodeficiency,...
...purchase below to continue the course
- Punctures, such as stab wounds, may involve little damage to the tissue on the skin surface, but may have more significant implications for or damage below the skin surface, including to internal organs. Patients with puncture wounds are also at risk for local infection, sepsis, and tetanus, thus requiring prophylactic treatment (Baddour & Brown, 2025). The Centers for Disease Control and Prevention (CDC) recommend that patients with contaminated wounds should have tetanus immune globulin and a tetanus vaccination if the patient does not have a clear history of prior tetanus vaccination or if vaccination did not occur within the last five years (Tiwari et al., 2024).
- Type I is a linear or flap tear that can be repositioned to cover the wound bed.
- Type II is partial tissue loss that cannot be repositioned to cover the wound bed.
- Type III involves total skin flap loss exposing the entire wound bed.
Figure 2
Wound Stage
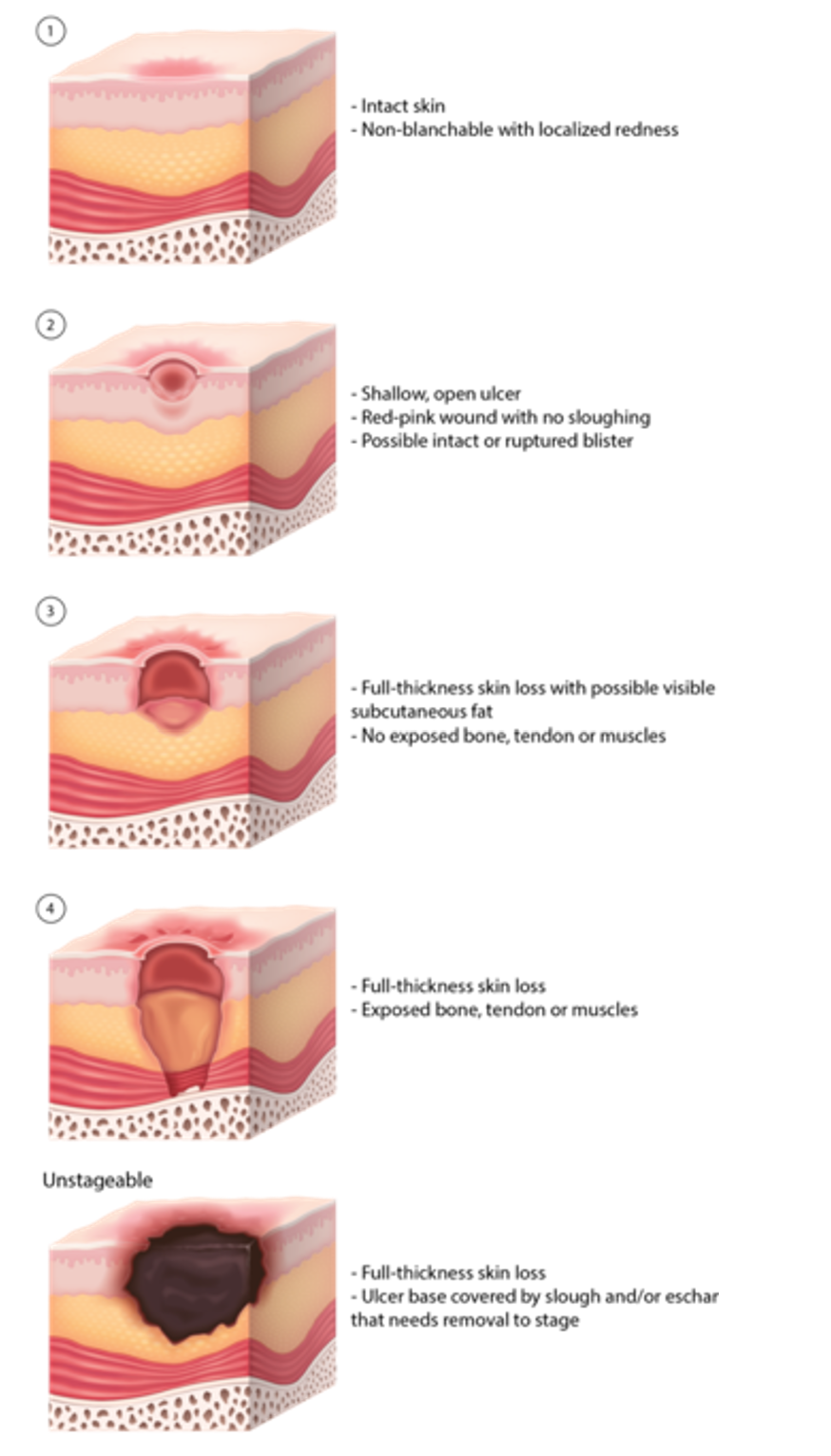
Table 1
| NPIAP Staging of Pressure-Induced Skin and Soft Tissue Injuries | |
| Stage | Description |
| 1 | Skin is intact but with non-blanchable redness for over 1 hour after relief of pressure. |
| 2 | Blister or other break in the dermis has partial thickness skin loss, with or without infection. Subcutaneous fat is not visible. |
| 3 | Full-thickness skin loss occurs, with or without infection. Subcutaneous fat may be visible. Undermining and tunneling may be present. |
| 4 | Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone, with or without infection—often includes undermining and tunneling. |
| Unstageable | Full-thickness skin and tissue loss occurs in which the base of the wound is covered by slough and/or eschar in the wound bed. |
| Deep Tissue Pressure Injury | There is localized, persistent, non-blanchable purple or maroon discolored but intact skin or blood-filled blister due to damage of underlying tissue from prolonged pressure or shear at the bone-muscle interface. |
NPIAP Staging of Pressure-Induced Skin and Soft Tissue Injuries
Stage Description
1 Skin is intact but with non-blanchable redness for over 1 hour after relief of pressure.
2 Blister or other break in the dermis has partial thickness skin loss, with or without infection. Subcutaneous fat is not visible.
3 Full-thickness skin loss occurs, with or without infection. Subcutaneous fat may be visible. Undermining and tunneling may be present.
4 Full-thickness skin and tissue loss occurs with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone, with or without infection—often includes undermining and tunneling.
Unstageable Full-thickness skin and tissue loss occurs in which the base of the wound is covered by slough and/or eschar in the wound bed.
Deep tissue pressure injury There is localized, persistent, non-blanchable purple or maroon discolored but intact skin or blood-filled blister due to damage of underlying tissue from prolonged pressure or shear at the bone-muscle interface.
For more information on pressure injuries, consult the Pressure Injuries Nursing CE course.
- Arterial or venous insufficiencies may cause ulcers due to impaired blood flow and decreased oxygenation. Venous ulcers result from venous hypertension and occur in the lower legs (refer to Figure 3). They account for approximately 85% of all leg wounds and are commonly found on the medial surface of the leg below the knee and above the ankle. These wounds usually have irregular borders, are red, and may have drainage. Arterial ulcers result from tissue ischemia caused by arterial insufficiency (refer to Figure 4). They occur at the most distal end of an arterial branch, most commonly in the feet. Arterial ulcers account for 5% to 20% of all leg ulcers. They can vary in color and appear pale or necrotic with a punched-out appearance, surrounded by edematous red skin. Arterial ulcers are often very painful for the patient (Mayrovitz et al., 2023).
Figure 3
Venous Ulcer

Figure 4
Peripheral Occlusive Arterial Disease

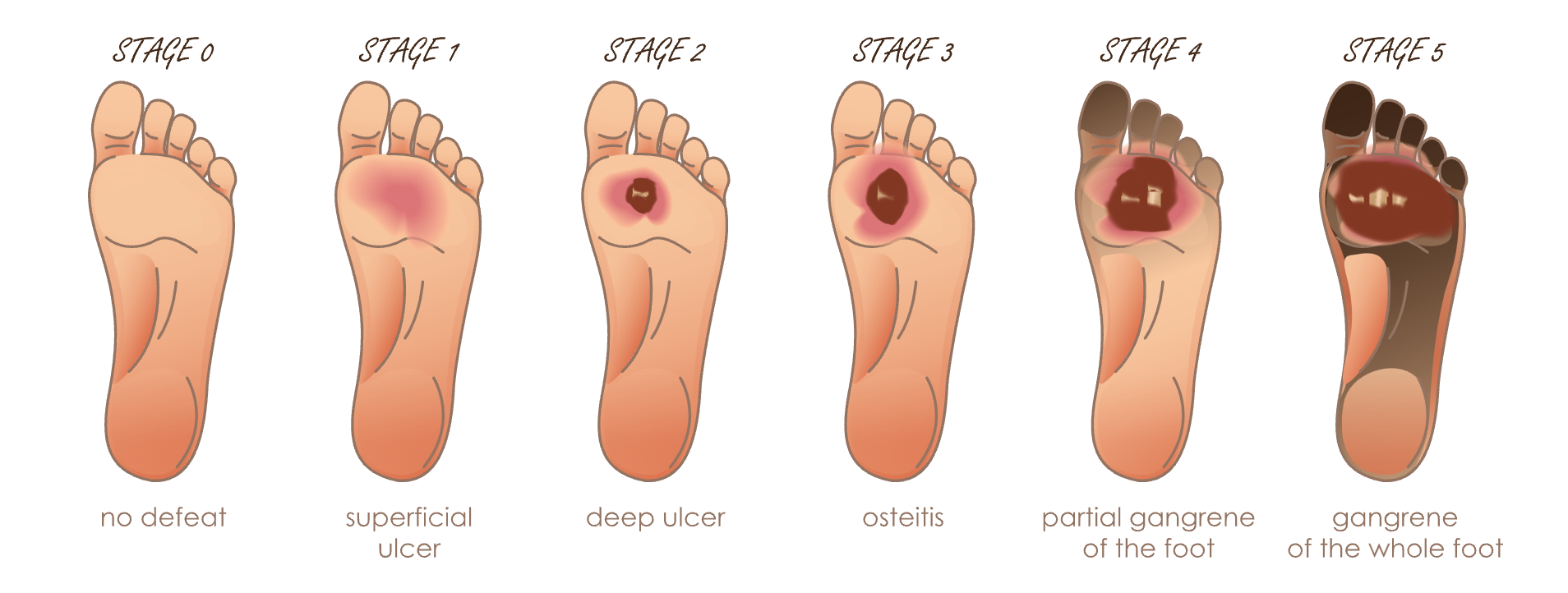
- Diabetic ulcers result from poor lower extremity circulation and neuropathies that result in decreased sensation (refer to Figure 5). They are a significant cause of morbidity and account for at least 66% of all nontraumatic surgical amputations in the United States. Infected or ischemic diabetic ulcers account for 25% of all hospitalizations of patients with diabetes. There are different staging systems, but the grade 1 through 5 system by Wagner is used often (Armstrong & de Asla, 2024).
Figure 5
Diabetic Foot Ulcer Staging
Developmental Implications
Infants and Children
Infants and children are at an increased risk of sustaining skin injuries due to their fragile skin. Although a full-term infant has anatomically similar skin to an adult, their dermal layer is half the thickness. Even though this thickness increases with age, the skin remains fragile throughout childhood until puberty. Skin injuries in children are more likely to be acute and caused by trauma (e.g., burn, scrape, or laceration); however, pediatric patients can develop chronic wounds from immobility or medical device use. Although children typically exhibit faster healing times, their decreased immune response, impaired thermoregulation, higher body surface-to-weight ratio, and elevated water loss through the transepidermal layer can put them at risk for delayed healing (Ciprandi et al., 2022; Dechant, 2022).
Postpartum
During pregnancy, the skin stretches and thins to accommodate the growing uterus. A pregnant individual may require an episiotomy during delivery or experience perineal tearing. An episiotomy is an incision made in the perineum by a healthcare provider (HCP). This is done to make the vaginal opening larger and prevent perineal tearing. Perineal tearing is similar to an episiotomy; however, it occurs naturally without the assistance of an HCP, resulting in jagged edges and making suturing more difficult. Once the baby is born, the incision from either an episiotomy or perineal tearing is sutured. Due to the proximity to stool and significant number of bacteria, dysfunctional healing can occur due to infections and dehiscence of surgical wounds, episiotomies, and perineal lacerations. These are common, occurring in up to a quarter of postpartum wounds (Berens, 2024; Berghella, 2024, 2025; Girsang & Elfira, 2023).
Older Adults
An older adult may have skin changes related to atrophy of the skin structures. As aging occurs, the skin loses its elasticity and starts to fold and sag. By the time an individual reaches their 70s or 80s, the skin is thinner, drier, and wrinkled. The epidermis thins and flattens, allowing for increased absorption of chemicals into the body. There is a decrease in elastin and collagen in the dermal layer, which increases the risk of skin tears and shearing injuries. Sweat and sebaceous glands decrease in number and leave the skin drier with an increased risk for heatstroke. Aging skin may have increased bruising from even mild trauma due to an increase in fragility of the vascular system. If an aging adult smokes tobacco or has sun exposure, the oxidative stress increases wrinkling, dryness, atrophy, and pigment changes, creating a leathery texture to the skin. The less melanated an individual's skin is, the more damage from sun and smoke exposure is visible. A wound in an older patient can take much longer to heal and carry a much higher associated risk than a similar wound in a younger patient (Hussein et al., 2024; National Institute on Aging, 2025).
Risk Factors
As noted previously, age can affect the healing process due to variations in skin structures and makeup. Further risk factors are related to comorbid conditions and disease processes, nutritional status (including obesity and malnutrition), medications, and tobacco or alcohol use. The nurse and the interdisciplinary team must recognize any underlying pathologies that impair wound healing. This includes assessments for underlying vascular impairment, neuropathy, metabolic disease, connective tissue disease, trauma, cancer treatment, iatrogenic disease, hospital-acquired infection, or an adverse effect of a medication that may affect the treatment plan (Armstrong & Meyr, 2023b). Each risk factor will be examined as follows.
Disease Processes
Diabetes Mellitus
Inadequate tissue perfusion and ischemia can occur when blood glucose is not controlled in patients with diabetes (either type 1 or type 2) and can hinder the wound healing process (WHP). This ischemia can prolong inflammation, leading to further tissue damage. Diabetes is also associated with a decreased immune response during wound healing. The patient may also be unaware of an injury to their feet or other body areas and continue to apply pressure to the area due to reduced sensation secondary to neuropathy that can occur because of uncontrolled diabetes. These untreated injuries allow bacterial infiltration. Diabetic wounds can be chronic and take months or years to heal, while others may never completely heal (Armstrong & de Asla, 2024; Rogers & Brashers, 2023; Weintrob, 2024; Wernick et al., 2023).
Infection
Bacteria are present on all skin surfaces and can enter a wound when the skin's integrity is breached. When the bacterial presence increases and wound damage occurs, an infection is present. Infection contributes to wound chronicity, morbidity, and mortality. Most wound infections occur from bacterial colonization. This can be from outside bacteria or an increase in the normal skin flora. The most common wound infections are caused by S. aureus and other types of staphylococci. Healthy individuals can usually avoid an infection due to their immune system's defense response, yet an immunocompromised patient will have a decreased ability to prevent an infection (Evans & Kim, 2024; Singhal, 2023). "The number of bacteria and their effect on the patient are categorized as: contamination, colonization, local infection, spreading infection, and systematic infection" (NPIAP, 2019, p. 251). Micro-organisms may multiply, invade, or damage tissues in or around the wound bed, delay healing, and cause systemic responses. Infection is present if a pressure injury is not healing due to bacteria in the wound bed. Chronic wounds may also develop biofilm, complex colonies of microbes encased in a protective extracellular polymer attached to the surface and embedded into the wound bed. Pseudomonas aeruginosa and S. aureus are the most common microbes in wound biofilms. Bacteria composing the biofilm are traditionally more challenging to treat. When a biofilm is present in the wound, the healing process stalls at the inflammatory phase and fails to progress to the proliferative and epithelialization stages. Biofilms must be removed by debridement and prevented from reforming with antiseptics and antimicrobial dressings (Evans & Kim, 2024; Gajula et al., 2020; NPIAP, 2019). Other signs or symptoms of infection are:
- Erythema that extends past the wound edges
- Induration of the tissue
- An increase or change in pain
- A change in temperature
- Purulent drainage
- An increase in wound size
- Systemic reactions including fever, malaise, lymph node enlargement, confusion, or anorexia (particularly in the older adult; Armstrong & Meyr, 2023b; NPIAP, 2019)
Immunodeficiency
The healing process may be impaired in those who are immunocompromised secondary to HIV infection, cancer, burns, or immunosuppressive therapies such as corticosteroids and chemotherapeutic drugs (refer to the section on medications). Other factors leading to immunodeficiency are age, malnutrition, recent surgery, significant trauma, liver cirrhosis, chronic renal disease, diabetes mellitus, and systemic lupus erythematosus. Stress can increase cortisol levels, blocking the production of cytokines and decreasing the immune response. Impairing or reducing the body's immune response negatively impacts wound healing (Armstrong & Meyr, 2023b; Gethin et al., 2022; Wernick et al., 2023).
Vascular Disease
Patients with PVD often have nonhealing wounds on the extremities. These wounds are chronic with delayed healing due to decreased blood flow depriving the area of sufficient oxygenation and the nutrients needed for adequate wound healing (Fukaya & O'Banion, 2025).
Dry Wound Bed
A dry wound bed can inhibit wound healing. Landmark evidence that moist wounds heal quicker was found in 1962. In a moist wound bed, the exudate (the moisture that seeps out of the wound site) transports enzymes, growth factors, and hormones into the wound bed. These mediators promote cellular communication and movement of the wound through the healing stages. In the absence of moisture, the cells involved in healing cannot move across the wound bed, the wound edges dry out, and epithelial cells fail to grow over the wound. Consequently, healing will stop, and necrotic tissue will form. A dry wound bed can also lead to dressing adherence, requiring interventions to remove the dressing and avoid damage to the wound bed. Too much exudate can impair wound healing; however, a moist wound bed is preferred over a dry one (Fletcher & Probst, 2020; Nuutila & Eriksson, 2021).
Nutrition
Elevated BMI
With an estimated 40% of adults in the United States with a BMI over 30, this clinical population has a high prevalence of wounds. Skin irritation and breakdown may occur in the presence of obesity. Pressure injuries can also affect this patient population. An elevated BMI may limit activity, body movement, and optimal blood flow. These limitations can lead to pressure injuries even when mobility is assisted. Patients with a BMI over 40 often require two or more individuals to reposition or assist them with activities of daily living (ADLs) in the home and clinical settings. If an individual with an elevated BMI is also incontinent, the risk of skin breakdown increases further. Micro-organisms grow in the moist skin folds and increase the risk of rashes and lesions. Poorly vascularized adipose tissue and greater skin surface area increase the risk of skin injury. An elevated BMI may also decrease vascularization, a significant factor in wound healing (Armstrong & Meyr, 2023b; Wernick et al., 2023).
Malnutrition
The nutritional needs required for proper wound healing are complex due to the increased demand for micronutrients and macronutrients. Because proteins are the building blocks of tissues, sufficient protein intake and amino acid–rich foods are needed to ensure proper wound healing. Individuals who are malnourished do not have adequate nutritional intake to promote proper wound healing. These individuals are also at an increased risk for developing pressure injuries due to decreased subcutaneous fat and more pronounced bony prominences (Ghaly et al., 2021; Wernick et al., 2023).
Medications
Certain medications can inhibit or interfere with the WHP, often by affecting a specific step in the process. Common medications that affect the WHP include the following.
- Corticosteroids affect wound healing through multiple mechanisms, including gene expression inhibition, suppression of many cellular wound responses, and anti-inflammatory effects. Corticosteroid therapy increases the risk for infection in wounds. They cause decreased fibroplasia and neovascularization, which thins the epidermis and significantly impacts wound healing when corticosteroids are given over a prolonged time.
- Anticoagulants such as warfarin (Coumadin), apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) inhibit coagulation factor production and disrupt the hemostasis phase of the WHP.
- Antibiotics such as erythromycin (Erythrocin) and gentamycin (Garamycin) can decrease inflammation or cause damage to cell membranes through the inhibition of protein synthesis. Although antibiotics are used to treat infection, they can delay wound healing through tensile strength reduction and effects on collagen cross-linking.
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil, Motrin) or celecoxib (Celebrex) have anti-inflammatory effects and inhibit platelet aggregation. The inhibition of prostaglandins and COX-1 interferes with healing and can increase hypoxia and ischemia of chronic venous ulcers.
- Dipeptidyl peptidase-4 Inhibitors (DDP-4 Inhibitors) such as vildagliptin (Galvus) and linagliptin (Tradjenta) can increase the risk for bullous pemphigoid or Stevens-Johnson syndrome. These wound-causing cutaneous diseases can develop due to the involvement of DDP-4 in immune pathways and wound healing.
- Chemotherapeutics agents such as capecitabine (Xeloda) and cyclophosphamide (Cytoxan) are associated with skin complications that can progress to ulcerations. Chemotherapeutic agents inhibit cellular metabolism, cellular division, or angiogenesis to stop the growth of cancer cells. Unfortunately, this therapeutic action also influences wound healing by decreasing the ability of skin to regenerate (Bennett et al., 2024; Oropallo, 2024).
Tobacco and Alcohol Use
Smoking/Vaping/Smokeless Tobacco
Tobacco use has a profound effect on the WHP. Multiple healing pathways are affected by tobacco use; however, ischemia is the major contributing factor to wound healing. The nicotine in cigarettes, vape pens, and smokeless tobacco (e.g., chew or dip) acts as a vasoconstrictor and stimulates the release of epinephrine. The release of epinephrine further reduces blood flow causing hypoxia. Nicotine also increases platelet adhesion and alters fibrinolysis, which causes the blood to become more viscous, leading to decreased blood flow. Tobacco use contributes to the development of chronic obstructive pulmonary disease (COPD), which chronically lowers the oxygen level in the blood. Cigarettes and vape pens also contain carbon monoxide, which has a 200-times higher affinity to hemoglobin than oxygen. Due to this increased affinity, even a small amount of carbon monoxide in the blood can profoundly impact the oxygen-carrying capability of hemoglobin, leading to less oxygen reaching the tissues. Patients who successfully cease smoking, vaping, or using smokeless tobacco show improved wound healing (Gethin et al., 2022; Wernick et al., 2023).
Alcohol
Alcohol use impacts all body systems, and the skin is equally affected. Alcohol disrupts the immune system and the WHP. Slow wound healing is more pronounced in individuals who binge drink or consume alcohol regularly. Not only does alcohol consumption slow wound healing, but it also increases the risk of acquiring a wound infection and delays the closure of both surgical and nonsurgical wounds. Alcohol impairs the production of collagen and impedes the inflammatory response, which plays a role in wound healing. “A one-time exposure to alcohol decreases wound angiogenesis by up to 61%” (Gethin et al., 2022, p. 28). Excessive alcohol use is associated with chronic malnutrition, further impairing wound healing. Adequate nutrition is vital for wound healing, and alcohol use inhibits the absorption of fat- and water-soluble vitamins such as A, B, C, D, E, and K. Deficiencies in these vitamins or proteins can impair wound healing (Gethin et al., 2022; Gramlich & Tandon, 2023).
Wound Healing and Closure
There are four stages of wound healing: hemostasis, inflammation, proliferation, and remodeling. The clotting cascade is initiated when a wound forms, whether due to trauma or a medical procedure. Platelets are the first to arrive in the area and release cytokines and growth factors, leading to hemostasis. This release of cytokines and growth factors promotes the migration of inflammatory cells to the wound. Within 24 to 48 hr after initial wound development, vasodilation occurs, allowing inflammatory cells, including neutrophils, monocytes, macrophages, and lymphocytes, to perform specialized functions within the injured tissue. Neutrophils arrive at the wound to phagocytize bacteria and clear microbial and cellular debris. The accumulation of macrophages occurs 48 to 72 hr after wound development, initiating the proliferation phase of the WHP. Macrophages further promote the inflammatory healing process by releasing additional cytokines, clearing cellular debris, and attracting blast cells to the wound. Then, fibroblasts begin to form the extracellular matrix (ECM) and allow for re-epithelialization of the wound as the proliferation phase transitions to the remodeling phase of the WHP. Endothelial cells promote angiogenesis and the formation of a new capillary bed to continue the remodeling process. Then, myofibroblasts promote wound contracture. Once fully healed, most wounds regain 70 to 80% of their original baseline tensile strength (Wernick et al., 2023).
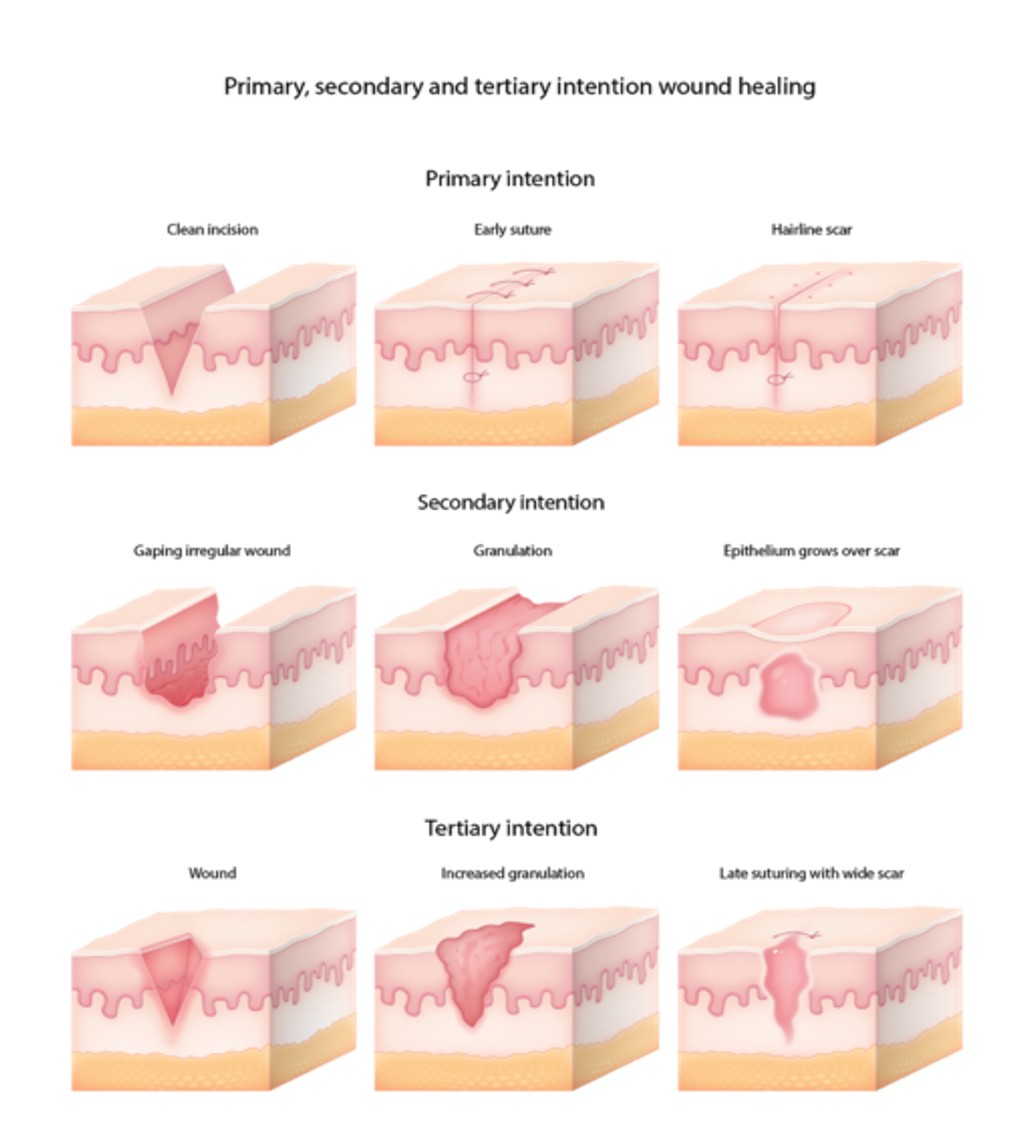
HCPs can implement different wound closure mechanisms to assist with the WHP. Various treatments are implemented based on the wound closure type. The following are wound closure options (refer to Figure 6).
- Primary-intention healing or primary closure occurs when wound edges are brought together and closed using staples or sutures. Surgical wounds or those with minimal tissue loss allow for primary closure and result in minimal scarring, assuming they are caused by sharp objects that are fairly clean.
- Secondary-intention healing or secondary closure occurs when a wound is left open for granulation tissue to form, contracting the wound edges and leading to epithelization. This type of closure is often used for burns or wounds too extensive for primary intention. Healing by secondary intention increases the risk of wound infection due to the lack of an epidermal barrier. Wounds that are typically allowed to heal by secondary intention are deep puncture or stab wounds that are unable to adequately be irrigated, grossly contaminated wounds, cavities with an abscess, wounds that present after a delay of greater than 24 hr, or animal bites in non-cosmetic regions.
- Tertiary-intention healing or delayed primary closure involves postponing the closure of a wound for a period of time. This period varies depending on the wound and HCP preference. These types of wounds usually do not have significant tissue loss but are often grossly contaminated. They can potentially be closed after exploration of the wound for foreign objects, irrigation, debridement, and observation for complications for three to seven days. Delayed primary closure is also appropriate for uncomplicated wounds that present after 24 hr (Azmat & Council, 2023; Brancato, 2025).
Figure 6
Types of Wound Healing
Nursing Assessment
Every patient who enters an acute care, home health, or long-term care setting should have a skin assessment within 24 hr of admission. This assessment should occur as soon as possible to ensure that all preexisting wounds are carefully identified, documented, and that appropriate treatment is initiated. An approved skin assessment risk tool should be utilized to identify preexisting injuries and determine the risk for pressure wound development during the inpatient or outpatient admission. This full, head-to-toe skin assessment is typically completed upon admission, upon transfer from a different unit or facility, with any condition change that may increase the patient's risk and repeated daily to identify skin changes early (NPIAP, 2019).
The Joint Commission (TJC, 2025) has included the prevention of hospital-acquired pressure injuries in their National Patient Safety Goals for acute and long-term care settings for years. This continues in the 2025 Patient Safety Goals. They suggest using a skin assessment tool such as the Braden Skin Assessment Scale. The Braden Skin Assessment Scale has been in use since 1988 and is the most used tool for assessing risk of pressure injuries and skin breakdown during hospitalizations or in long-term care facilities (Huang et al., 2021; TJC, 2022). The Braden Skin Assessment Scale estimates a patient's risk of pressure injuries by assessing the factors described in Table 2.
Table 2
Braden Skin Assessment Scale
Sensory Perception | 1. Completely Limited: Unresponsive (does not moan, flinch, or grasp) to painful stimuli due to diminished level of consciousness or sedation. OR Limited ability to feel pain over most of body surface. | 2. Very Limited: Responds only to painful stimuli. Cannot communicate discomfort except by moaning or restlessness. OR Has a sensory impairment that limits the ability to feel pain or discomfort over half of body. | 3. Slightly Limited: Responds to verbal commands but cannot always communicate discomfort or need to be turned. OR Has some sensory impairment that limits ability to feel pain or discomfort in one or two extremities. | 4. No Impairment: Responds to verbal commands; has no sensory deficit that would limit ability to feel or voice pain or discomfort. |
| Moisture Degree to which skin is exposed to moisture | 1. Constantly Moist: Skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time patient is moved or turned. | 2. Very Moist: Skin is often, but not always, moist. Linen must be changed at least once a shift. | 3. Occasionally Moist: Skin is occasionally moist, requiring an extra linen change approximately once a day. | Rarely Moist: Skin is usually dry; linen only requires changing at routine intervals. |
| Activity Degree of physical activity | 1. Bedfast: Confined to bed. | 2. Chairfast: Ability to walk severely limited or nonexistent. Cannot bear weight and/or must be assisted into chair or wheelchair. | 3. Walks Occasionally: Walks occasionally during day, but for very short distances, with or without assistance. Spends majority of each shift in bed or chair. | 4. Walks Frequently: Walks outside the room at least twice a day and inside room at least once every two hours during waking hours. |
| Mobility Ability to change and control body position | 1. Completely Immobile: Does not make even slight changes in body or extremity position without assistance. | 2. Very Limited: Makes occasional slight changes in body or extremity position, but unable to make frequent or significant changes independently. | 3. Slightly Limited: Makes frequent though slight changes in body or extremity position independently. | 4. No Limitations: Makes major and frequent changes in position without assistance. |
| Nutrition Usual food intake pattern | 1. Very Poor: Never eats a complete meal. Rarely eats more than one-third of any food offered. Eats two servings or less of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement. OR Is NPO and/or maintained on clear liquids or IVs for more than five days. | 2. Probably Inadequate: Rarely eats a complete meal and generally eats only about one-half of any food offered. Protein intake includes only three servings of meat or dairy products per day. Occasionally will take a dietary supplement. OR Receives less than optimum amount of liquid diet or tube feeding. | 3. Adequate: Eats over half of most meals. Eats a total of four servings of protein (meat, dairy products) each day. Occasionally will refuse a meal but will usually take a supplement if offered. OR Is on a tube feeding or TPN regimen, which probably meets most of nutritional needs. | 4. Excellent: Eats most of every meal. Never refuses a meal. Usually eats a total of four or more servings of meat and dairy products. Occasionally eats between meals. Does not require supplementation. |
| Friction and Shear | 1. Problem: Requires moderate to maximum assistance in moving. Complete lifting without sliding against sheets is impossible. Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance. Spasticity, contractures, or agitation lead to almost constant friction. | 2. Potential Problem: Moves feebly or requires minimum assistance. During a move skin probably slides to some extent against sheets, chair, restraints, or other devices. Maintains relatively good position in chair or bed most of the time but occasionally slides down. | 3. No Apparent Problem: Moves in bed and in chair independently and has sufficient muscle strength to lift completely during move. Maintains good position in bed or chair at all times. | |
(Agency for Healthcare Research and Quality, 2014, section 3D; Bergstrom et al., 1987)
Each category is given a score of 1 to 4 (except the friction and shear category, which is scored 1 to 3). These scores are then added together to determine the individual's risk for skin-related issues during admission. Total scores may range from 6 to 23. The higher the score, the lower the risk of pressure injuries. A score of 18 or less indicates an increased risk for developing a pressure injury. After the patient's risk has been determined, interventions are instituted accordingly to prevent the development of skin breakdown (Bergstrom et al., 1987; Hovan 2021; NPIAP, 2019).
After completing the risk assessment tool and identifying any preexisting wounds, the nurse must perform a focused wound assessment to determine the plan of action. The initial step is taking a thorough history, including any risk factors that may impede the healing process. Considerations for the initial history include systemic diseases such as diabetes and PVD, smoking history, alcohol use, medications (e.g., NSAIDs, corticosteroids, anticoagulants, chemotherapeutics, and antiplatelets), nutrition, and any other factors that may impact healing. Additionally, the nurse will assess the origin of the wound, onset of injury or awareness of the wound, and any recent changes related to the wound, including increasing pain, drainage, or severity (Armstrong & Meyr, 2023b; Gethin et al., 2022).
Determining the origin of a wound is an essential part of the assessment to predict further complications that may occur. Other factors that should be considered are the location, depth, size, age of the injury, and pain level. Wound healing complications may increase based on any of these factors. A careful assessment of the wound and documentation to share with the healthcare team will offer insight into the healing process and allow for early intervention if a change in treatment is needed (Armstrong & Meyr, 2023b; Nagle et al., 2023).
The wound bed and surrounding tissue must be assessed for size and depth in centimeters. The measuring device is most often a disposable tool to avoid contamination. Mobile applications have been found to be more accurate but are not as widely utilized. The width is measured at the longest distance across the wound, and the length at a 90-degree angle to the width. Most HCPs use the clock method to determine the reference points, such as "12 and 6, 3 and 9" for length and width. To measure the depth of a wound, a cotton-tipped swab can be inserted into the deepest part of the wound and the distance where it meets the skin edges marked. Then, the distance from the end of the swab to this mark is measured to determine the wound depth. HCPS should avoid pushing into the wound bed as organs or vessels could be injured. A picture of the wound is often suggested for insurance reimbursement and to track healing progress. Before taking photos of wounds, consent for photography should be obtained to avoid HIPAA or Health Information Technology for Economic and Clinical Health (HITECH) violations. Facility policies regarding wound care photography acquisition should be followed (Alder, 2025a, 2025b; Health Quality Innovation Network [HQIN], n.d.; NPIAP, 2019).
In addition to measurements, a clear description of the wound appearance is vital. The wound bed tissue description should include color, tissue type, surrounding tissue condition, edge appearance, and the presence or absence of moisture or a dry wound bed. The color and odor of drainage should be described if present. In contrast, too much moisture can be equally detrimental and damage the intact cells at the wound's edge. HCPs must monitor the wound edges to ensure the skin is smooth without rolled or dry edges. The color of the wound bed and the surrounding skin can indicate concerns. White skin surrounding the wound indicates too much moisture. Erythema or inflammation can indicate infection, injury, tape burn, or irritation from wound care products. Typically, infection is indicated by erythema, edema, pain, fluctuance, malodor, and purulent drainage (Bowers & Franco, 2020; Nagle et al., 2023).
The tissue around the wound should be palpated to determine whether it is hard or soft, as indurated tissue can indicate infection or inflammation. Any areas of hardness or induration should be measured and documented. A wound bed tissue assessment should include appropriate terminology for the wound bed condition, including the presence of granulation tissue, fibrin slough, or eschar (Evans & Kim, 2024; HQIN, n.d.).
Diagnosing Wounds
An interdisciplinary team must diagnose the patient's wound and initiate appropriate evidence-based care. Upon discovery, nurses should thoroughly investigate a wound to help determine if the cause is pressure, friction, or traumatic injury. In addition, diagnostic testing may be done to determine the optimum treatment plan. Testing could include lab work to evaluate the patient's nutritional status (albumin and prealbumin) or potential infection, imaging studies (e.g., ultrasound, doppler, x-ray) to assess any underlying injuries, or biopsy as appropriate (Armstrong & Meyr, 2023a; Nagle et al., 2023).
Treatments
Wound treatment will vary depending on the nature of the injury and individual patient factors. For example, an older adult with diabetes who has a pressure injury on their foot will be managed differently than a younger, otherwise-healthy patient with the same wound. Treatment options vary in cost, availability, and accessibility, so careful consideration should be taken to determine the best treatment modality in collaboration with the interdisciplinary team. Both topical and systemic antimicrobial agents may be used in conjunction with dressings (Bergstrom et al., n.d.; CDC, 2025a).
Wound Cleansing
Wound cleansing will vary across wound types but can be a vital part of the WHP as an opportunity to remove foreign materials, necrotic tissue, excess medication, and bacteria or contamination. Unless contraindicated, wound cleansing should occur with each dressing change. Typical wound cleansing is completed with normal saline, sterile water, or a commercial cleanser with varying ingredients. Cleansers should be hypoallergenic, nontoxic to the healthy tissue, and appropriate to use with any intended dressings. All manufacturer guidelines for dressing products should be followed (Armstrong & Meyr, 2024b).
Antibiotics
If antibiotics/antimicrobials are to be used, a wound culture should be obtained first to identify the causative organism, promote treatment effectiveness, and reduce the risk of antibiotic-resistant organisms. The CDC (2025a) lists seven pathogens found in healthcare settings that are antimicrobial resistant. Infections with antimicrobial-resistant organisms increased 20% in hospital settings during the COVID-19 pandemic and have remained at that level since plateauing in 2022. This spike is most likely due to longer hospital stays and inappropriate antibiotic use (CDC, 2025a). CDC reports from 2019 revealed that over 2.8 million infections and 35,000 deaths in the United States were due to antibiotic-resistant organisms created by the overuse of antibiotic therapies (Amin et al., 2023). Antimicrobial stewardship programs focus on infection prevention, appropriate antimicrobial use (correct antibiotic at the correct time for the correct duration), and the use of evidence-based standards and guidelines for antibiotic prescriptions. Antibiotic treatment should be used only when needed and limited to the shortest effective duration. Testing should be completed to rule out underlying disease processes. Antimicrobial therapies should be discontinued once the wound infection clears, and inflammation has improved. Wound dressings coated with dialkylcarbamoyl chloride (DACC) can be used to reduce the bacterial burden within wounds and delay or prevent the need for antibiotic use. If a biofilm is recognized, a tissue biopsy may be necessary. Other healthcare team members should be notified of signs and symptoms of infection, including dieticians, nurses, and providers, such as vascular and wound care specialists. Poor nutritional status, lack of glycemic control, certain medications, and inadequate circulation may contribute to infection. Any deficits in these areas should be further explored and managed by the healthcare team (CDC, 2025a; NPIAP, 2019; Rippon et al., 2021).
Treatment of infected wounds can include systemic antibiotics, topical antiseptics, silver Silvadene, medical-grade honey, or topical antibiotics (NPIAP, 2019). Wound dressings should be selected based on the following.
- Ability to keep the wound bed moist
- Need to address the bacterial burden
- Type and amount of wound exudate
- Condition of the tissue in the wound bed
- Status of the surrounding skin
- Injury stage and location
- Presence of tunneling or undermining
- Goals of the patient and the healthcare team (Britto et al., 2024; NPIAP, 2019)
Antibiotic therapy is indicated for wounds that are more severe than a local, superficial infection. Therapy includes intravenous (IV) and/or oral antibiotics to elicit systemic effects. Topical antibiotic use should be limited to situations in which the benefits outweigh the risks of side effects and bacterial resistance. For mild infections without signs of systemic involvement, amoxicillin-clavulanate (Augmentin) plus either trimethoprim-sulfamethoxazole (Bactrim) or doxycycline (Vibramycin) would be appropriate. If amoxicillin-clavulanate (Augmentin) is not feasible due to allergy or intolerability, levofloxacin (Levaquin) can be used instead. For more severe infections with systemic involvement, parenteral regimens are preferred, such as vancomycin (Vancocin) plus ceftazidime (Fortaz) or cefepime (Maxipime) plus metronidazole (Flagyl), which can be given orally due to high bioavailability. Alternative options include a carbapenem such as meropenem (Merrem) plus vancomycin (Vancocin). Pseudomonal coverage can be ensured with ciprofloxacin (Cipro), levofloxacin (Levaquin), ceftazidime (Fortaz), cefepime (Maxipime), or meropenem (Merrem). Most patients can be switched to oral therapy once a clinical response (resolution of systemic signs and symptoms) is observed. Specific side effects of antibiotics are dependent on their administration route and classification. General side effects of IV antibiotics include swelling, redness, and pain at the injection site. Common side effects of oral antibiotics include diarrhea, nausea, bloating, and abdominal pain (NPIAP, 2019; Singhal, 2021; Tleyjeh & Berlowitz, 2024).
Debridement
Wound debridement removes all material from the wound that is impeding healing. This includes necrotic tissue, cellular debris, exudate, bacteria, and foreign materials. The goal of debridement is to promote re-epithelialization. Debridement is used for various types of wounds, including pressure injuries and burns (Evans & Kim, 2024; Manna et al., 2023; Mayer et al., 2024). There are a variety of debridement methods, including autolytic, enzymatic, mechanical, surgical, and biological debridement.
- Autolytic debridement is the most gentle, conservative type of debridement and uses the body's enzymes and healing processes to rehydrate, soften, liquefy, and then expel the necrotic tissue from the wound. Occlusive dressings are often used to keep the body's fluids in the wound bed and maintain a moist healing environment, such as absorptive hydrofibers, alginate dressings, hydrocolloid dressings, and amorphous hydrogel. This is not recommended in infected wounds, those that need to be urgently debrided, or wounds with large amounts of necrotic tissue, undermining, or tunneling. Immunocompromised patients should not undergo autolytic debridement (Avila-Rodríguez et al., 2020; Manna et al., 2023; Nowak et al., 2022).
- Enzymatic debridement, or chemical debridement, is the process of dissolving necrotic tissue, cellular debris, wound exudate, and foreign materials. One commonly used medication in this category is collagenase (Santyl) ointment. The active ingredient is from the bacterium Clostridium histolyticum, which breaks down collagen in necrotic tissue. This debridement can also be used on burns to remove eschar. Patients with wounds that are heavily infected are not candidates for this treatment. Products with silver and Dakin solution are contraindicated for use in conjunction with collagenase (Avila-Rodríguez et al., 2020; Manna et al., 2023; Mayer et al., 2024; Nowak et al., 2022).
- Surgical debridement is performed by a physician or primary HCP. Surgical debridement physically removes necrotic tissue, cellular debris, wound exudate, or eschar from the wound bed to facilitate healing. This invasive procedure uses sharp and sterile instruments to excise nonviable materials from the wound bed. For wounds requiring this intervention, the interdisciplinary team must support the procedure and perform subsequent wound care and assessments. Nonhealing or inadequately perfused wounds should not be surgically debrided as this may lead to further complications, including necrosis or enlargement of the wound bed. Surgical debridement can be quite painful and appropriate pain management should be part of the treatment plan (Manna et al., 2023; Mayer et al., 2024).
- Mechanical debridement removes exudate, necrotic or infected material, and foreign bodies from the wound bed. After cleansing a wound, a wet-to-dry dressing (i.e., gauze pads soaked in saline) can be applied to the wound bed. After the dressing has dried, it is removed. The goal is to pull away the top layer of tissue within the wound with the dried dressing. The disadvantage of a wet-to-dry dressing is that it is nonselective; the entire top layer of the wound is removed without discerning between viable and nonviable tissue. A 2024 international consensus document on debridement best practices determined that this method should be the last choice when no alternative was available due to the associated pain and harm. Debridement pads are preferred over traditional gauze pads. Other methods of mechanical debridement that are recommended include hydrotherapy, pulsatile lavage, ultrasonic debridement, and negative pressure wound therapy and instillation with dwell time (NPWTi-d; Manna et al., 2023; Mayer et al., 2024).
- Hydrosurgical debridement is performed in an operating room (OR) with a high-power waterjet and suction. In comparison to moist dressings, hydrotherapy debridement is well tolerated by patients who are sensitive to pain. It is faster and more selective than a blade with a straight edge. It can also be done at the bedside with a micro waterjet, and special training is not required.
- Pulsatile lavage combines intermittent lavage with suction to loosen and remove nonviable tissue from the wound bed. Although this is fast and effective, caution must be taken not to damage underlying structures such as blood vessels, bones, and tendons. Pulsatile lavage is also costly because the equipment is single use only.
- Ultrasonic debridement uses low- or high-frequency ultrasonic waves that create acoustic energy to remove nonviable tissue from the wound bed. When used in conjunction with standard wound care, ultrasonic debridement can safely and effectively remove necrotic tissue and promote wound healing. This type of debridement is extremely helpful with cavity wounds.
- NPWTi-d is a mechanical debridement technique that uses a reticulated open-cell foam (ROCF) that combines the instillation of normal saline or other solution with a foam that has mechanical debriding effects. It is a gentle wound-healing approach that can be useful for patients who are unable to tolerate sharp/surgical debridement.
Mechanical debridement can be excruciating for the patient, so premedication with analgesics is indicated to increase patient comfort. Patients on anticoagulant medications or with underlying coagulopathy may have significant bleeding with mechanical debridement, so these individuals require extra caution and care (Manna et al., 2023; Mayer et al., 2024).
- Biologic debridement, otherwise known as maggot debridement therapy, uses sterile, medical-grade larvae of the Lucilia sericata species of the greenbottle blowfly to remove necrotic tissue from a wound bed. This type of debridement is used for chronic wounds, including diabetic foot ulcers, venous stasis ulcers, pressure injuries, and burns. It is beneficial for large wounds needing painless removal of necrotic tissue. Proteolytic enzymes are released from the larvae and dissolve necrotic tissue. The wound bed should first be cleaned, and sterile larvae are then applied to the wound and covered with a mesh-like, air-permeable dressing for one to three days; the dressing and larvae are then removed. If further debridement is needed, the process can be repeated. Wounds should never be allowed to close over the larvae, and they should not be left in the wound bed if they die, as this increases the risk of allergic reaction or infection. Used larvae are considered contaminated and should be disposed of properly by sealing them in a plastic bag and placing the bag in a biohazard container for incineration (Manna et al., Nowak et al., 2022; Thomas et al., 2021; Wernick et al., 2023).
Skin Grafting
Skin grafts promote the healing of extensive burns, wounds, and venous or pressure injuries (refer to Figure 7). They may also be performed to restore skin that has been removed during surgery or after a severe skin infection. Grafts taken from the patient's body (an autograft) have the lowest risk of rejection. Grafts may also be taken from a cadaver, an animal, or created using synthetic tissue. Grafts should be placed on tissue that will support growth and adherence. Grafts placed on bone, tendons, or nerves will likely be unsuccessful as there is a limited blood supply to support the growth of the graft. Wounds with necrotic tissue, eschar, or high bacterial counts also do not support graft success. Factors that increase graft complications include patient age (very young or older patients), smoking, diabetes, poor overall health, and certain medications. There are three types of graft techniques: split-thickness grafts, full-thickness grafts, and composite grafts. Depending on the method, healing time may vary. Skin graft procedures can be painful, so anesthesia is administered to prevent pain during the surgery. Pain control after the procedure can be managed with oral, intramuscular (IM), or IV pain medication. Skin tissue engineering is a newer procedure that uses stem cells to produce skin products that can replace damaged tissue (Vecin & Kirsner, 2023).
Figure 7
Skin Graft

Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy (HBOT) can be used on chronic wounds to promote wound healing. Wounds that are not healing are typically hypoxic, and increasing oxygen tension and pressure by various methods can stimulate healing. HBOT promotes muscle and nerve regeneration by stimulating angiogenesis or developing new blood vessels. The treatments can be done on limbs placed in a limb-encasing device or a full-body chamber. HBOT has been in use for over 40 years and should be part of an interdisciplinary team approach with a comprehensive plan of care for wound healing that includes strategies for extensive vessel disease, glycemic abnormalities, nutritional deficiencies, infection, and the presence of necrotic tissue. Relative contraindications for systemic HBOT are asthma or COPD, claustrophobia, recent ear or thoracic surgery, eustachian tube dysfunction, asymptomatic pulmonary blebs or bullae noted on chest radiographs, seizure history, and upper respiratory infections. Medications could also have potential adverse effects with conjunctive use, such as bleomycin (Blenoxane) and doxorubicin (Rubex), but evidence is sparse. An untreated pneumothorax is the only absolute contraindication to HBOT (Manaker, 2024; Wernick et al., 2023).
Negative-Pressure Wound Therapy
Negative-pressure wound therapy (NPWT), also called vacuum-assisted wound closure, applies suction or negative pressure to the wound bed. This promotes wound healing by removing excess drainage, stimulating vascularization, and supporting the closure of wound edges or margins. Negative pressure creates mechanical stress that promotes growth factor expressions, angiogenesis, and granulation tissue growth. The negative pressure opens the capillary beds and draws blood to the wound area, reduces edema and bacterial colonization, and provides a moist wound bed. This treatment is most often used on deep or full-thickness wounds and chronic wounds such as pressure injuries and diabetic foot ulcers. It can also be used to prepare a wound bed for skin grafting. Pain is commonly reported as an adverse reaction and should be proactively managed during treatment. This treatment should not be used in wounds with vital structures that are exposed or tissue that is malignant. Caution is advised in patients who have ischemic wounds, infectious wounds, devitalized tissue or fragile skin, an allergy to adhesives, or an increased risk of bleeding as life-threatening hemorrhage could result (Gestring, 2025; Wernick et al., 2023).
Dressings
A proper dressing will support wound healing and accelerate the healing time. Dressing types will likely change throughout the healing stages, and the HCP will need to assess the injury and adjust the type of dressing throughout the trajectory of care. Unfortunately, the cost is essential to determine wound care products when planning treatment. Comfort and usability are important factors to consider, as the patient or their family members may be performing the wound care once the patient is discharged from the healthcare facility. The frequency of dressing changes should also be considered, regarding staff workload and patient compliance. Newer treatment modalities require less frequent changes and can stay in place for extended periods with optimal results (Weller et al., 2020).
- Gauze and non-woven dressings have been used for wound care for decades and are inexpensive, but with the advancement of new materials designed to accelerate healing, they are rarely used in modern-day wound care. Daily dressing changes are required with these materials to manage drainage effectively. Gauze can be helpful in packing deep wounds in early stages (Britto et al., 2024; Mayer et al., 2024; Raju et al., 2022).
- Absorptive or superabsorbent dressings are made up of materials that will allow for optimal absorbency and may be used alone or in combination with other dressings. These dressings are typically cotton, cellulose, or rayon and absorb drainage to avoid tissue maceration. They are designed to be nonadherent and minimize damage to the wound bed or pain upon removal. These dressings are not appropriate for dry wound beds as they can cause further damage. Examples of absorptive dressings are Biatain Super Absorbent Dressing, ConvaMax Superabsorber Dressing, Covaderm, or Drawtex (Wound Source, n.d.).
- Alginates are used for highly exudative wounds and contain alginic acid from seaweed covered in calcium/sodium salts. These dressings are highly absorbent (up to 20 times their weight). Alginate dressings may also contain controlled-release ionic silver. These dressings interact with sodium ions to form a hydrophilic gel in the wound bed. They support a moist wound environment, absorb well, and may prevent microbial contamination. These dressings are used for pressure injuries, diabetic wounds, venous wounds, tunneling or cavity wounds, and wounds with minor bleeding. They are not recommended for use in wounds with anaerobic infections. Examples of alginate dressings are Algisite, Curasorb, Tegaderm Alginate, or Kaltostat (Weller et al., 2020).
- Skin substitutes are made to mimic human skin and are helpful for hard-to-heal wounds and burns. Skin substitutes protect the wound from further trauma and water loss and provide a physical barrier to bacteria while promoting new tissue growth and wound healing. They are further differentiated as class I (temporary dressings of impervious materials), class II (one layer of skin substitutes that are durable), and class III (permanent layers of composite materials). They also improve the functional and cosmetic results of the WHP, enhancing the quality of life for patients with wounds on exposed skin. Examples of skin substitutes are Dermagraft, DermACELL, and AlloPatch (Vecin & Kirsner, 2023).
- Bioactive dressings improve wound healing and are derived from natural sources, proteins, or tissues. These products are beneficial for burns and hard-to-heal wounds. Examples are collagen dressings and medical-grade honey (Wood, 2024).
- Hydrocolloid dressings are moisture-retentive dressings used to protect wounds with a small to moderate amount of drainage. These are often used to treat noninfected stage I through IV pressure injuries, partial- to full-thickness wounds, abrasions, and necrotic wounds. Hydrocolloids can function as a secondary dressing with alginates or wound fillers that need to remain in the wound bed for an extended time. Hydrocolloids should not be used on wounds with excessive exudate or to cover enzymatic debriding agents, gels, or ointments. Examples of hydrocolloid dressings are DuoDerm or Hydrocoll (Weller et al., 2020).
- Foam dressings can be constructed from either foam that draws in fluid and physically expands as it retains the drainage or pseudo-foam that contains absorbent materials such as viscose and acrylate fibers designed to hold extra fluid. These are best for wounds with moderate to heavy drainage. They can be used as a primary or secondary dressing on wounds and remain in place for up to seven days. Most are nonadhesive and can easily be used on those with allergies to adhesives. Antimicrobial foam dressings can be used on infected wounds. Examples of foam dressings are Tegafoam and Mepilex (Weller et al., 2020).
- Hydrogel dressings contain a high water/glycerin content within a gel base and are used to provide moisture to the wound bed. A moist environment facilitates the debridement of necrotic tissue and tissue granulation. The amorphous hydrogel can be applied in a layer over the wound surface, or a hydrogel-impregnated gauze can be used to fill dead spaces in deep wounds. These dressings should not be used for wounds with moderate to heavy exudate or when the goal of care is to maintain dry eschar. Hydrogel dressings can contain allergens such as iodine, silver, or sodium carboxymethyl cellulose and should not be used for patients with known sensitivities or allergies to these products. These dressings should not be combined with collagenase (Santyl) ointment because the iodine and silver may decrease the enzymatic action of the collagenase (Santyl). Examples of hydrogel dressings are Hydrosorb or Solugel (Medscape, n.d.; NPIAP, 2019; Weller et al., 2020).
- Hydrofiber and sodium carboxymethyl cellulose dressings are used for wounds that may require packing because they are available in sheets or ribbons. These products combine with the wound exudate to produce a hydrophilic gel that maintains a moist wound environment. These dressings should not be used on dry wounds. Examples of hydrofiber dressings are Exufiber and Aquacel (Weller et al., 2020).
- Hydroactive dressings are made up of multiple layers of polymers, including a contact layer that is non-adhesive and an absorbent foam. Like foam dressings, they are highly absorbent but have a different mechanism for absorption of exudate. They bring fluid into the polymer structure and hold the exudate, creating a moist environment as opposed to the syphon effect of foams. They allow drainage to flow through and reduce the risk of maceration. They may be used on burns, wounds with large amounts of exudate, pressure injuries, and lower extremity venous ulcers. They are nonadherent and protect the wound from bacteria. Examples of hydroactive dressings are Biatain surface sheets, Tielle surface sheets, and PolyMem surface sheets (Weller et al., 2020).
- Antimicrobial dressings are essential for routine care for an infected wound, particularly diabetic ulcers. These dressings decrease the number of bacteria in the wound bed and reduce the need for systemic antibiotics. The antimicrobial materials may be impregnated into other dressing types such as hydrogels or foams to reduce the bacterial count in the wound. Care must be used to choose the appropriate antimicrobial dressing that will support wound healing. Their use should be limited to short durations to avoid tissue damage or the development of resistant organisms. Examples of antimicrobial dressings include Actisorb, Aquacel Ag, Acticoat, Iodoflex, and Iodasorb (Yousefian et al., 2023). These dressings should not be combined with collagenase (Santyl) ointment because some antimicrobial formulations decrease the enzymatic action of the collagenase (Santyl; Medscape, n.d.).
- Semipermeable film dressings can be used to secure other wound care products or alone for clean, dry wounds with minimal drainage. These dressings allow for visualization of the wound and work well on areas that need to be waterproofed. They also use the body's fluids to support debridement. Film dressings should not be used on wounds with moderate to large amounts of drainage. Examples of film dressings are OpSite and Tegaderm (Weller et al., 2020).
While this is one list of dressing types and examples, it is by no means exhaustive of the vast resources for wound care. The nurse and interdisciplinary team must consider all aspects of each patient's needs and resources and determine the best plan of action in collaboration with the patient.
Nutrition
Nutrition is a fundamental requirement of the human body for typical day-to-day function. Patients with wounds have higher nutritional needs than healthy patients. Wound healing is complex and relies on the coordination and internal regulation of various metabolic processes to promote epithelialization within the injured tissue. Nutritional factors should be considered for all diseases, and intake should be optimized to promote the best outcomes. An optimal diet for those with a wound is high in protein and amino acids with sufficient amounts of vitamin A, vitamin B complex, vitamin C, vitamin E, iron, zinc, copper, fats, and carbohydrates. An early referral to a dietician can facilitate an appropriate dietary intake to support wound healing, and should be considered for any patient at risk of nutritional imbalances or deficiencies due to comorbidities such as diabetes, renal disease, obesity, liver disease, or any condition that affects the body's ability to process or eliminate nutrients (Armstrong & Meyr, 2023a, 2023b; Ghaly et al., 2021; Kangal & Regan, 2023).
The traditional recommendation on macronutrient amounts for an adult diet is 40 to 60% carbohydrates, 25 to 30% fat, and 15 to 20% protein, but patients with wounds should consume up to 250% more protein. This provides the body with the nutrients required for timely wound healing in most patients. Supplements may be needed to support the nutritional needs of some patients during the WHP, and dieticians and primary HCPs may collaborate to develop an ideal treatment plan that ensures adequate dietary intake (Ghaly et al., 2021).
Pain Control
Pain is an often-overlooked aspect of wound care, and many patients report that the pain they endure during wound care is as significant as the initial injury. Depending on the type and location of the wound, pain may or may not be a significant problem. Burns are particularly painful and require ongoing pain relief. Factors that increase pain include the depth of the wound, the structures involved, infection, and other injuries or conditions that coexist with the wound. The nurse should complete a pain assessment to determine all aspects of the patient's pain, including its location, exacerbating and relieving factors, quality, and severity, using a patient-appropriate pain scale. Premedicate with analgesics before debridement or other wound care that may incite pain. The HCP must time medication administration according to the expected onset of action and duration to ensure coverage during dressing changes or debridement (Admassie et al., 2022; Brown, 2023; Mayer et al., 2024; NPIAP, 2019). There are also nonpharmacologic interventions that the HCP can use to reduce pain and increase patient comfort during wound care activities.
- Distractions can help decrease pain, including watching television, deep breathing, listening to music, playing games, or reading a book.
- The HCP should provide education and information about wound care activities.
- The HCP should space out care to give the patient uninterrupted rest time in a quiet environment.
- Music therapy or other guided imagery techniques may reduce anxiety.
- The patient should be positioned for comfort during any procedures or dressing changes.
- Dressings should be soaked at least 30 min prior to removal.
- When possible, the number of dressing changes should be limited by using dressings that can remain in place for more extended periods.
- Dressing types, tapes, and adhesives that do not adhere to the wound bed or pull at the wound should be utilized whenever possible.
- The patient should be allowed to choose times for treatments or dressing changes whenever possible to create a feeling of independence or control and decrease anxiety (Admassie et al., 2022; Brown, 2023; NPIAP, 2019).
Sutures, Staples, and Surgical Glue
Sutures are the gold-standard method for closing minor surgical wounds or accidental injuries. In either situation, the nurse must monitor the suture line for approximation of the skin, signs of infection, and appropriate healing. Suture materials have changed substantially in the past decade, and wound closures may have many appearances. Suturing and staples are painful for the patient and require local or another form of anesthesia before the procedure. Most suture materials are synthetic and may be absorbable or nonabsorbable. Types must be differentiated so that proper instructions are given to the patient for follow-up care. Deep wounds may require multiple layers of sutures to minimize skin tension and reduce the risk of hematoma formation. Superficial sutures enable functional closure with minimal scarring for cosmetic purposes on areas like the face (Azmat & Council, 2023; deLemos, 2024).
Staples are typically used for superficial wounds. They are a reasonable alternative to sutures on the scalp and extremities. They are quick to insert, which is helpful in cases of brisk bleeding or mass casualty incidents. Staples are not suitable for areas such as the face due to poor cosmetic results. There is less risk of infection associated with staples because they do not form a tract between the wound edges. Most staples are made of stainless steel or titanium and should not interfere with an MRI. Still, if other injuries are suspected, a radiologist should be consulted to ensure there will be no interference from the staples or to assess whether another closure option would be best (Azmat & Council, 2023; Lipsett, 2023a).
Surgical adhesives/glues are highly effective in closing wounds in pediatric settings, where fear of needles is significant. Surgical glue is quick to apply and provides excellent cosmetic outcomes. Wound margins must be opposable and dry, which may not be the case with traumatic injuries. Glues work well for scalp wounds with fewer cosmetic complications reported (Azmat & Council, 2023; Lipsett, 2023b).
Vaccination
Contaminated wounds or those that are not sterile (e.g., bites, puncture wounds, skin tears, abrasions, or lacerations) can result in exposure to the bacteria Clostridium tetani. Tetanus is caused by the exotoxin produced by this bacterium. This leads to serious nervous system effects such as tightening of the jaw muscles, making it hard to breathe, open the mouth, or swallow. Tetanus is not contagious but is contracted via deep puncture wounds or cuts. Patients with burns or dead skin are also at risk (Thwaites, 2025; Tiwari et al., 2024).
The CDC has recommended that babies and children receive the diphtheria, tetanus, and acellular pertussis (DTaP) vaccine at 2, 4, and 6 months and boosters at 15 to 18 months and 4 to 6 years of age. Preteens and teens should get one dose of the tetanus, diphtheria, and pertussis (Tdap) vaccine between 11 and 12 years. Pregnant patients should have a Tdap vaccination during their third trimester of each pregnancy, and adults should have a tetanus booster (Td) every ten years. Patients who are injured and not current with their tetanus vaccination or who have never been vaccinated against tetanus must be given a Td booster for immediate protection (Tiwari et al., 2024).
Although not common, HIV may be transmitted through bites. Prophylaxis with antiretroviral treatments should be administered to decrease the chance of HIV transmission. This regimen includes multiple drugs used in combination to prevent replication, production, and the virus's ability to use host tissues (CDC, 2025b).
Rabies can be transmitted via animal bites. If the animal's infection status cannot be confirmed, rabies immune globulin and rabies vaccine should be administered as soon as possible after the initial injury. If a rabies infection is identified, the local and national health departments should be notified of a risk to the general animal and human population (CDC, 2024).
Prevention
Bites
Animal bites are a significant cause of morbidity and mortality worldwide. Dog bites account for millions of injuries worldwide annually, with the highest risk being to children. Children and adults should be taught safe practices around animals to avoid bites, which include the following.
- Do not handle, pet, or feed unknown animals.
- Spay or neuter pets to decrease aggressiveness.
- Avoid leaving children unattended with animals, even family pets.
- All household animals should be vaccinated for rabies and other infectious diseases per state guidelines.
- Avoid tall grassy areas and wear protective footwear.
- Seek treatment immediately if an animal bites a child or adult, or if any signs of infection occur (Medline Plus, n.d.; World Health Organization, 2024).
Burns
Burns can be prevented by educating the public to do the following:
- Turn off electrical currents before attempting home repairs.
- Stand at least three feet away from hot outdoor objects (e.g., a grill or fire).
- Keep outlets covered with protective childproof coverings if small children are in the home.
- Repair or discard frayed electrical wires immediately.
- Keep water heater temperatures below 48.89 C (120 F).
- Avoid wearing loose-fitting clothing while cooking.
- Turn pot handles away from the front of the stove and keep children away from the burners of a hot stove.
- Keep hot drinks away from the edge of tables and counters.
- Do not allow appliance cords to dangle over the counter edge.
- Do not use heated blankets or pads while sleeping (American Burn Association, n.d.; Ready.gov, 2023; UpToDate., n.d.).
Pressure Injuries
Pressure injuries are entirely preventable with good nursing care and an interdisciplinary team focused on nutrition, activity, and proper hygiene (NPIAP, 2019). Nursing care for patients who are immobile or physically impaired due to an acute or chronic illness should include the following.
- Turning patients every two hours, unless contraindicated
- Keeping skin clean and dry at all times
- Keeping bed linens free of wrinkles and dry at all times
- Performing daily skin assessments or more frequently if the patient is incontinent
- Utilizing appropriate pressure relief devices, including mattress toppers, specialty mattresses, pillows, and wedges
- Integrating wound care experts into the interdisciplinary team if any areas of breakdown occur
- Consulting dietary/nutrition services to ensure proper nutrition
- Utilizing incontinence products if indicated (e.g., barrier creams for prophylaxis in the inpatient setting at any sign of erythema [NPIAP, 2019])
Skin Tears
The International Skin Tear Advisory Panel (ISTAP) defines skin tears as "a traumatic wound caused by mechanical forces, including removal of adhesives" (Wogamon-Harmon, 2022, para. 1). Nursing staff should focus on preventing skin tears, especially in older adults. The following strategies advised by ISTAP can be implemented to prevent skin tears.
- Identify and remove potential sources of injury, including medical equipment, through a comprehensive risk assessment.
- Initiate fall prevention measures such as adequate lighting, especially in unfamiliar environments like a hospital.
- Apply padding to beside rails, wheelchair armrests, and leg supports.
- Encourage patients to wear long sleeves and pants when the weather allows.
- Keep caregiver and patient fingernails smooth and short.
- Encourage good nutrition and hydration.
- Apply moisturizing creams frequently to prevent dry skin.
- Avoid placing products with adhesive directly onto the skin; if necessary, use paper tape and non-adhesive dressings.
- Use skin guards for individuals who repeatedly experience skin tears (Wogamon-Harmon, 2022).
Diabetic Ulcers
Patients with diabetes should be educated on preventative measures to decrease the risk of developing a diabetic ulcer. Nurses should teach all clients the following.
- Encourage patients to control their blood glucose level by eating a healthy diet, monitoring their blood glucose regularly, maintaining an exercise regimen, and taking all medications as prescribed.
- Patients should visit their primary HCP annually and as needed.
- Patients should visit their physician or podiatrist for inspections and regular care of their feet. This may vary but should be done annually. Patients at high risk may need to have their toenails cut by a podiatrist to prevent complications.
- Patients or caregivers should perform daily foot inspections.
- Patients should wear shoes that fit well.
- Patients should be instructed to keep the area between their toes dry and avoid applying lotion to this area.
- Encourage patients to wear cotton socks and footwear when walking (Wernick et al., 2023; Wexler, 2024).
Vascular Ulcers
Both venous and arterial disorders can lead to ulcers. However, venous ulcers are present in up to 40% of lower extremity wounds (Armstrong & Meyr, 2023b; Criqui et al., 2021). The following strategies should be taught to all patients with peripheral artery disease or PVD.
- Glycemic control with diabetes
- Daily inspection of feet, especially in between toes and soles of feet
- Smoking cessation
- Moderate exercise (after consulting with an HCP)
- Routine health check-ups
- Medication compliance (anticoagulants, antihypertensives, and statins) as prescribed (Criqui et al., 2021; Fukaya & O'Banion, 2025)
Wound Care Specialty Certifications and Organizations
While all nurses are expected to deliver safe and effective care to patients with wounds, there are higher-level certifications for those wishing to demonstrate expertise in this area. Nurses certified in wound care offer their patients a higher level of care and add credibility to their organization. The following organizations certify and support nurses who specialize in wound care.
- The Wound, Ostomy, and Continence Nursing Society (WOCN, 2022) offers the Wound, Ostomy, and Continence (WOC) certification.
- The National Alliance of Wound Care and Ostomy (NAWCO, n.d.) offers the Wound Care Certification (WCC).
- The American Board of Wound Management (ABWM, n.d.) offers the Certified Wound Specialist (CWS) and Certified Wound Care Associate (CWCA) certifications for nurses.
References
Admassie, B. M., Ferede, Y. A., Tegegne, B. A., Lema, G F., & Admass, B. A. (2022). Wound-related procedural pain management in a resource limited setting: Systematic review. International Journal of Surgery Open, 47, 100549. https://doi.org/10.1016/j.ijso.2022.100549
Agency for Healthcare Research and Quality. (2014). Preventing pressure ulcers in hospitals. https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/index.html
Alder, S. (2025a). What are the HIPAA photography rules? The HIPAA Journal. https://www.hipaajournal.com/hipaa-photography-rules/
Alder, S. (2025b). What Is the HITECH Act? The HIPAA Journal. https://www.hipaajournal.com/what-is-the-hitech-act/
American Board of Wound Management. (n.d.). Certification resources. Retrieved March 3, 2025, from https://abwmcertified.org/certification-resources/
American Burn Association. (n.d.). Prevention resources. Retrieved March 3, 2025, from https://ameriburn.org/prevention/prevention-resources/
Amin, V. P., Dhanani, M., Patel, J., Dhawan, A., Mahesh, G., Chenna, V. S. H., Kyada, S., Dekhne, A., & Desai, H. D. (2023). Burden of bacterial antimicrobial resistance in United States in 2019: A systematic analysis. Open Forum Infectious Diseases, 10(Suppl 2), ofad500.1855. https://doi.org/10.1093/ofid/ofad500.1855
Armstrong, D. G., & de Asla, R. J. (2024). Management of diabetic foot ulcers. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/management-of-diabetic-foot-ulcers
Armstrong, D. G., & Meyr, A. J. (2023a). Clinical assessment of chronic wounds. UpToDate. Retrieved March 5, 2025, from https://www.uptodate.com/contents/clinical-assessment-of-chronic-wounds
Armstrong, D. G., & Meyr, A. J. (2023b). Risk factors for impaired wound healing and wound complications. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/risk-factors-for-impaired-wound-healing-and-wound-complications
Armstrong, D. G., & Meyr, A. J. (2024a). Basic principles of wound healing. UpToDate. Retrieved March 3, 2025, from https://uptodate.com/contents/basic-principles-of-wound-healing
Armstrong, D. G., & Meyr, A. J. (2024b). Principles of acute wound management. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/principles-of-acute-wound-management
Avila-Rodríguez, M. I., Meléndez-Martínez, D., Licona-Cassani, C., Aguilar-Yañez, J. M., Benavides, J., & Lorena Sánchez, M. (2020). Practical context of enzymatic treatment for wound healing: A secreted protease approach (Review). Biomedical Reports, 13(1), 3–14. https://doi.org/10.3892/br.2020.1300
Azmat, C. E., & Council, M. (2023). Wound closure techniques. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470598/
Baddour, L. M., & Brown, A. M. (2025). Infectious complications of puncture wounds. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/infectious-complications-of-puncture-wounds
Baddour, L. M., & Harper, M. (2024). Animal bites (dogs, cats, and other mammals): Evaluation and management. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/animal-bites-dogs-cats-and-other-mammals-evaluation-and-management
Barrett, J. (2024). Human bites. Medscape. https://emedicine.medscape.com/article/218901-overview
Bennett, G., Abbott, J., & Sussman, G. (2024). The negative impact of medications on wound healing. Wound Practice and Research, 32(1), 17–24. https://doi.org/10.33235/wpr.32.1.17-24
Berens, P. (2024). Overview of the postpartum period: Disorders and complications. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/overview-of-the-postpartum-period-disorders-and-complications
Berghella, V. (2024). Cesarean birth: Surgical technique. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/cesarean-birth-surgical-technique
Berghella, V. (2025). Cesarean birth: Postoperative care, complications, and long-term sequelae. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/cesarean-birth-postoperative-care-complications-and-long-term-sequelae
Bergstrom, N., Braden, B. J., Laguzza, A., & Holman, V. (1987). The Braden Scale for predicting pressure sore risk. Nursing Research, 36(4), 205–210. https://pubmed.ncbi.nlm.nih.gov/3299278/
Bergstrom, N., O’Harra, P., & Foster, W. M. (n.d.). Collaborative interdisciplinary teams and pressure injury prevention. American Nurse Today. Retrieved March 3, 2025, from https://americannursetoday.mydigitalpublication.com/publication/?i=492685&article_id=3075067&view=articleBrowser&ver=html5
Berlowitz, D. (2023). Clinical staging and general management of pressure-induced skin and soft tissue injury. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/clinical-staging-and-general-management-of-pressure-induced-skin-and-soft-tissue-injury
Bowers, S., & Franco, E. (2020). Chronic wounds: Evaluation and management. American Family Physician, 101(3), 159–166. https://www.aafp.org/pubs/afp/issues/2020/0201/p159.html
Brancato, J. C. (2025). Minor wound evaluation and preparation for closure. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/minor-wound-evaluation-and-preparation-for-closure
Britto, E. J., Nezwek, T. A., Popowicz, P., & Robins, M. (2024). Wound dressings. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK470199/
Brown, A. (2023). Assessing and managing wound pain. Practice Nursing, 34(1). https://www.practicenursing.com/content/clinical-focus/assessing-and-managing-wound-pain
Centers for Disease Control and Prevention. (2024). Rabies post-exposure prophylaxis. https://www.cdc.gov/rabies/hcp/prevention-recommendations/post-exposure-prophylaxis.html
Centers for Disease Control and Prevention. (2025a). Antimicrobial resistance threats in the United States, 2021–2022. https://www.cdc.gov/antimicrobial-resistance/data-research/threats/update-2022.html
Centers for Disease Control and Prevention. (2025b). Clinical guidance for PEP. https://www.cdc.gov/hivnexus/hcp/pep/
Ciprandi, G., Crucianelli, S., Grussu, F., Spuntarelli, G., Marino, S. F. M., Urbani, U., Paola, B., Sisto, A., Rizzo, M. I., & Zama, M. (2022). Meeting challenges in pediatric wound care: Our 15-year experience with dialkylcarbamoyl chloride-coated dressing technology in acute and chronic wounds. Chronic Wound Care Management and Research, 9, 23–33. https://doi.org/10.2147/CWCMR.S376889
Criqui, M. H., Matsushita, K., Aboyans, V., Hess, C. N., Hicks, C. W., Kwan, T. W., McDermott, M. M, Misra, S., & Ujueta, F. (2021). Lower extremity peripheral artery disease: Contemporary epidemiology, management gaps, and future directions: A scientific statement from the American Heart Association. Circulation, 144, e171–e191. https://doi.org/10.1161/CIR.0000000000001005
Dechant E. D. (2022). Considerations for skin and wound care in pediatric patients. Physical medicine and rehabilitation clinics of North America, 33(4), 759–771. https://doi.org/10.1016/j.pmr.2022.06.009
deLemos, D. M. (2024). Skin laceration repair with sutures. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/skin-laceration-repair-with-sutures
Evans, K., & Kim, P. J. (2024). Overview of treatment of chronic wounds. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/overview-of-treatment-of-chronic-wounds
Fletcher, J., & Probst, A. (2020). Managing dry wounds in clinical practice: Challenges and solutions. Wounds International, 11(2), 47–52. https://woundsinternational.com/journal-articles/managing-dry-wounds-clinical-practice-challenges-and-solutions/
Fukaya, E., & O'Banion, L. A. (2025). Evaluation and management of chronic venous insufficiency Including venous leg ulcer. UpToDate. Retrieved March 10, 2025, from https://www.uptodate.com/contents/evaluation-and-management-of-chronic-venous-insufficiency-including-venous-leg-ulcer
Gajula, B., Munnamgi, S., & Basu, S. (2020). How bacterial biofilms affect chronic wound healing: A narrative review. International Journal of Surgery Global Health, 3(2), e16. https://doi.org/10.1097/GH9.0000000000000016
Gestring, M. (2025). Negative pressure wound therapy. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/negative-pressure-wound-therapy
Gethin, G., Touriany, E., Van Netten, J. J., Sobotka, L., & Probst, S. (2022). The impact of patient health and lifestyle factors on wound healing, part 1: Stress, sleep, smoking, alcohol, common medications and illicit drug use. Journal of Wound Management. Official Journal of the European Wound Management Association. https://doi.org/10.35279/jowm2022.23.01.sup01.01
Ghaly, P., Iliopoulos, J., & Ahmad, M. (2021). The role of nutrition in wound healing: An overview. British Journal of Nursing, 30, (5). https://www.britishjournalofnursing.com/content/nutrition/the-role-of-nutrition-in-wound-healing-an-overview/
Girsang, B. M., & Elfira, E. (2023). A literature review on postpartum perineal wound care: Epidemiology, impact, and future Interventions. Open Access Macedonian Journal of Medical Sciences, 11(F), 73-80. https://doi.org/10.3889/oamjms.2023.11073
Gramlich, L., & Tandon, P. (2023). Nutritional status in patients with sustained heavy alcohol use. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/nutritional-status-in-patients-with-sustained-heavy-alcohol-use
Health Quality Innovation Network. (n.d.). Wound measurement & documentation guide. Retrieved March 4, 2025, from https://hqin.org/wp-content/uploads/2021/06/Wound-Measurement-Documentation-Guide.pdf
Hovan, H. (2021). Understanding the Braden Scale: Focus on sensory perception (Part 1). Wound Source. https://www.woundsource.com/blog/understanding-braden-scale-focus-sensory-perception-part-1
Huang, C., Ma, Y., Wang, C., Jiang, M., Yuet Foon, L., Lv, L., & Han, L. (2021). Predictive validity of the Braden Scale for pressure injury risk assessment in adults: A systematic review and meta-analysis. Nursing Open, 8(5), 2194–2207. https://doi.org/10.1002/nop2.792
Hussein, R. S., Dayel, S. B., Abahussein, O., & El-Sherbiny, A. A. (2024). Influences on skin and intrinsic aging: Biological, environmental, and therapeutic insights. Journal of Cosmetic Dermatology, (24)2, e16688. https://doi.org/10.1111/jocd.16688
Kangal, M. K. O., & Regan, J. P. (2023). Wound healing. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK535406/
The Joint Commission. (2022). Quick safety issue 25: Preventing pressure injuries (updated March 2022). https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/quick-safety/quick-safety-issue-25-preventing-pressure-injuries/
The Joint Commission. (2025). National patient safety goals. https://www.jointcommission.org/standards/national-patient-safety-goals/
Lipsett, S. (2023a). Closure of minor skin wounds with staples. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/closure-of-minor-skin-wounds-with-staples
Lipsett, S. (2023b). Minor wound repair with tissue adhesives (cyanoacrylates). UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/minor-wound-repair-with-tissue-adhesives-cyanoacrylates
Manaker, S. (2024). Hyperbaric oxygen therapy. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/hyperbaric-oxygen-therapy
Manna, B., Nahirniak, P., & Morrison, C. A. (2023). Wound debridement. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK507882/
Mayer, D. O., Tettlebach, W. H., Ciprandi, G., Downie, F., Hampton, J., Hodgson, H., Lazaro-Martinez, J. L., Probst, A., Schultz, G., Stürmer, E. K., Parnham, A., Frescos, N., Stang, D., Holloway, S., & Percival, S. L. (2024). Best practice for wound debridement. Journal of Wound Care, 33(Sub6b), S1-S32. https://doi.org/10.12968/jowc.2024.33.Sup6b.S1
Mayrovitz, H. N., Wong, S., & Mancuso, C. (2023). Venous, arterial, and neuropathic leg ulcers with emphasis on the geriatric population. Cureus, 15(4), e38123. https://doi.org/10.7759/cureus.38123
Medline Plus. (n.d.) Animal bites. Retrieved March 4, 2025, from https://medlineplus.gov/animalbites.html
Medscape. (n.d.). Collagenase (Rx). Retrieved March 3, 2025, from https://reference.medscape.com/drug/santyl-collagenase-343561#0
Mikel, G., Bliss, D. Z., & McNichol, L. (2022). Moisture-associated skin damage, expanding and updating practice based on the newest ICD-10-CM codes. Journal of Wound, Ostomy and Continence Nursing, 49(2), 143–151. https://doi.org/10.1097/WON.0000000000000865
Nagle, S. M., Stevens, K. A., & Wilbraham, S. C. (2023). Wound assessment. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482198/
National Alliance of Wound Care and Ostomy. (n.d.). Wound care certified certification - WCC. Retrieved March 4, 2025, from https://www.nawccb.org/wound-care-certification
National Institute on Aging. (2025). Skin care and aging. https://www.nia.nih.gov/health/skin-care/skin-care-and-aging#
National Pressure Injury Advisory Panel. (2019). Prevention and treatment of pressure ulcers/injuries: Clinical practice guideline. https://static1.squarespace.com/static/6479484083027f25a6246fcb/t/6553d3440e18d57a550c4e7e/1699992399539/CPG2019edition-digital-Nov2023version.pdf
Nowak, M., Mehrholz, D., Barańska-Rybak, W., & Nowicki, R. J. (2022). Wound debridement products and techniques: Clinical examples and literature review. Advances in Dermatology and Allergology, 39(3), 479–490. https://doi.org/10.5114/ada.2022.117572
Nuutila, K., & Eriksson, E. (2021). Moist wound healing with commonly available dressings. Advances in Wound Care, 10(12), 685–698. https://doi.org/10.1089/wound.2020.1232
Oropallo, A. (2024). Overview of the care of adult patients with nonhealable wounds. UpToDate. Retrieved March 10, 2025, from https://www.uptodate.com/contents/overview-of-the-care-of-adult-patients-with-nonhealable-wounds
Raju, N. R., Silina, E., Stupin, V., Manturova, N., Chidambaram, S. B., & Achar, R. R. (2022). Multifunctional and smart wound dressings-A review on recent research advancements in skin regenerative medicine. Pharmaceutics, 14(8), 1574. https://doi.org/10.3390/pharmaceutics14081574
Ready.gov. (2023). Preventing and treating burns. https://www.ready.gov/preventing-and-treating-burns
Rice, P. L., & Orgill, D. P. (2024). Assessment and classification of burn Injury. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/assessment-and-classification-of-burn-injury
Rippon, M. G., Rogers, A. A., & Ousey, K. (2021). Antimicrobial stewardship strategies in wound care: Evidence to support the use of dialkylcarbamoyl chloride (DACC)-coated wound dressings. Journal of Wound Care, 30(4). https://doi.org/10.12968/jowc.2021.30.4.284
Rogers, J. L. and Brashers, V. L. (Eds.). (2023). McCance and Huether's pathophysiology: The biologic basis for disease in adults and children (9th ed.). Elsevier.
Shrestha, R., Krishan, K., Ishaq, H., Kanchan, T. (2023). Abrasion. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK554465/
Singer, A. J. (2022). Abrasions. MSD Manual Professional Version. https://www.msdmanuals.com/professional/injuries-poisoning/lacerations-and-abrasions/abrasions
Singhal, H. (2023). Wound infection medication. Medscape. https://emedicine.medscape.com/article/188988-medication#2
Thomas, D. C., Tsu, C. L., Nain, R. A., Arsat, N., Fun, S. S., & Sahid Nik Lah, N. A. (2021). The role of debridement in wound bed preparation in chronic wound: A narrative review. Annals of Medicine and Surgery (2012), 71, 102876. https://doi.org/10.1016/j.amsu.2021.102876
Thwaites, L. (2025). Tetanus. UpToDate. Retrieved March 5, 2025, from https://www.uptodate.com/contents/tetanus
Tiwari, T. S. P., Moro, P. L., & Acosta, A. M. (2024). Chapter 21: Tetanus. Center for Disease Control and Prevention. https://www.cdc.gov/pinkbook/hcp/table-of-contents/chapter-21-tetanus.html
Tleyjeh, I. M., & Berlowitz, D. (2024). Infectious complications of pressure-induced skin and soft tissue injury. UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/infectious-complications-of-pressure-induced-skin-and-soft-tissue-injury
UpToDate. (n.d.). Patient education: Electrical burns (the basics). Retrieved March 3, 2025, from https://www.uptodate.com/contents/electrical-burns-the-basics
Vecin, N. M., & Kirsner, R. S. (2023). Skin substitutes as treatment for chronic wounds: Current and future directions. Frontiers in Medicine, 10, 1154567. https://doi.org/10.3389/fmed.2023.1154567
Weintrob, A. C. (2024). Diabetic foot Infection, Including osteomyelitis: Clinical manifestations and diagnosis. UpToDate. Retrieved March 3, 2025, from https://www.uptodate.com/contents/diabetic-foot-infection-including-osteomyelitis-clinical-manifestations-and-diagnosis
Weller, C. D., Team, V., & Sussman, G. (2020). First-line interactive wound dressing update: A comprehensive review of the evidence. Frontiers in Pharmacology, 11, 155. https://doi.org/10.3389/fphar.2020.00155
Wernick, B., Nahirniak, P., & Stawicki, S. P. (2023). Impaired wound healing. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK482254/
Wexler, D. J. (2024). Patient education: Foot care for people with diabetes (beyond the basics). UpToDate. Retrieved March 4, 2025, from https://www.uptodate.com/contents/foot-care-for-people-with-diabetes-beyond-the-basics
Wogamon-Harom, C. L. (2022). Skin tears: Causes, prevention, and treatment. Wound Source. https://www.woundsource.com/blog/skin-tears-causes-prevention-and-treatment
Wood, B. (2024). Skin grafts and biologic skin substitutes. Medscape. https://emedicine.medscape.com/article/1295109-overview
World Health Organization. (2024). Animal bites. https://www.who.int/news-room/fact-sheets/detail/animal-bites
Wound, Ostomy, and Continence Nurses Society. (2022). Become a WOC nurse. https://www.wocn.org/page/become_a_woc_nurse
Wound Source. (n.d.). Specialty absorptives/specialty absorbents. Retrieved March 3, 2025, from https://www.woundsource.com/product-category/dressings/specialty-absorptives-super-absorbents
Yousefian, F., Hesari, R., Jensen, T., Obagi, S., Rgeai, A., Damiani, G., Bunick, C. G., & Grada, A. (2023). Antimicrobial wound dressings: A concise review for clinicians. Antibiotics, 12(9), 1434. https://doi.org/10.3390/antibiotics12091434