About this course:
This learning activity aims to increase nurses' knowledge regarding the minimum acceptable standards of safe, effective nursing practice for a registered nurse (RN), licensed practical nurse (LPN), or advanced practice registered nurse (APRN) in any setting in Ohio as outlined in Chapter 4723 of the Ohio Revised Code (ORC) and Chapters 4723-1 through 4723-27 of the Ohio Administrative Code (OAC).
Course preview
Ohio Category A Nursing CE Course: Intro to the Nurse Practice Act for Initial Licensure
This learning activity aims to increase nurses' knowledge regarding the minimum acceptable standards of safe, effective nursing practice for a registered nurse (RN), licensed practical nurse (LPN), or advanced practice registered nurse (APRN) in any setting in Ohio as outlined in Chapter 4723 of the Ohio Revised Code (ORC) and Chapters 4723-1 through 4723-27 of the Ohio Administrative Code (OAC).
Upon completion of this activity, learners should be able to:
- describe the origin and purpose of regulatory bodies such as boards of nursing (BON)
- summarize the Ohio Board of Nursing's (OBN) standards of practice for RNs, LPNs, and APRNs
- outline the OBN Scope of Practice Decision-Making Model
- list the steps in the OBN's disciplinary process and discuss the OBN's most recent annual reports
- define the steps for license renewal and continuing professional development requirements in the Ohio Nurse Practice Act
- explore the process and parameters for nurse delegation and supervision within the ORC Chapter 4723.67
Nursing education and practice standards result from nursing associations' efforts dating back over 100 years. Nursing regulatory bodies (NRBs), also referred to as state boards of nursing (BONs), were established to regulate nursing practice in all 50 states, the District of Columbia, and 4 US territories. The governments in these states and territories created NRBs to protect the public and ensure they receive quality and safe nursing care. This is achieved by establishing the standards of safe nursing care, the scope of practice, and disciplinary guidelines known as the Nurse Practice Act (NPA). The NPA designates the BON, or the authoritative body within each state, to ensure the nursing workforce delivers safe, competent, skilled, and knowledgeable care. The NRBs also establish the requirements that must be met for an individual to obtain licensure to practice. Once a license is issued to an individual, it remains the duty of the NRB to monitor these individuals and ensure compliance with the established standards of care. When a nurse demonstrates unsafe nursing practice and deviates from the established standards of care, the NRB determines disciplinary action. All NRBs in the US are members of the National Council of State Boards of Nursing (NCSBN, n.d.-a).
This course explores the Ohio NPA standards outlined in Chapter 4723 of the Ohio Revised Code (ORC) to protect the public and to ensure that minimum competencies and requirements are met and maintained by all nurses. The ORC comprises laws passed by the state of Ohio legislative bodies. The Ohio Administrative Code (OAC) is an adjunct document outlining the rules adopted by various agencies throughout Ohio to carry out the laws passed by the general assembly. OAC 4723 is relevant to the BON and is divided into 27 chapters. These chapters outline the initial licensure and renewal regulations, standards of practice, disciplinary actions, and requirements for pre-licensure nursing education (OBN, n.d.-b; The Ohio Legislature 136th General Assembly, n.d.). This training will focus primarily on the OAC.
| For the most recent copy of the Ohio NPA, please visit the OBN’s website. |
History of Boards of Nursing
In 1896 the American Nurses Association (ANA) was established to make nursing a recognized profession with established standards to regulate practice. As the ANA gained traction and nursing became recognized as a formal profession in the early 20th century, the need arose for the creation of regulatory bodies or nursing boards to enforce newly passed laws and set professional standards. In 1903, North Carolina became the first state to establish a BON. Soon afterward, many states enacted similar legislation and established their own BON. As more BONs were established and professional standards were set, licensing became common and eventually mandatory in 1935. With this mandate, the titles of RN and LPN became protected legally, only referring to those who had gained state licensure (Graduatenursing.edu, n.d.).
Structure of the Ohio Board of Nursing
The structure of the OBN is specified in ORC 4723.02. The OBN comprises 13 members who must be US citizens and residents of Ohio. Eight members must be RNs (i.e., graduates of an accredited nursing school) with an active license in Ohio. These individuals must have been actively engaged in nursing practice as an RN for the 5 years immediately preceding their initial appointment to the board. Of the eight RNs on the board, at least two must hold a current, valid license issued by the OBN to practice as an advanced practice registered nurse (APRN, which includes certified nurse-midwife [CNM], certified nurse practitioner [CNP], certified registered nurse anesthetist [CRNA], and clinical nurse specialist [CNS]). Four members must be LPNs who graduated from an accredited education program and hold an active license in Ohio. These individuals must have been actively engaged in nursing practice as an LPN for the 5 years immediately preceding their initial appointment to the OBN. One consumer member is appointed to represent the interest of individuals who receive care from nurses licensed by the state. This individual, or any of their immediate family members, must not have a financial stake in health care delivery or be associated with a particular health care profession (ORC, 2017a).
Board members serve 4-year terms beginning on January 1 and ending on December 31. When an individual's term expires, a qualified candidate with the same nursing license is chosen as their successor. When selecting board members, the disbursement throughout Ohio is considered to ensure fair representation of all geographical areas throughout the state. The Ohio governor may remove any individual from the board who is unable or unwilling to meet the position's requirements during their term. This includes neglecting duties or engaging in unprofessional behavior. In this circumstance, a new member will be selected to fill the vacancy. When an individual takes over the term before expiration, they hold that position until the term is complete. Nursing organizations within Ohio can submit nominations to fill vacancies to the governor. However, with input from...
...purchase below to continue the course
Standards of Practice
The OBN can enforce and expand on state statutes through its written rules. Additionally, the OBN has the authority to conduct investigations and to impose discipline when a licensee violates a law or regulation. The minimally acceptable standards of safe and effective practice for the RN and LPN can be found in Chapters 4723-4-03 and 4723-4-04 of the OAC (2024a, 2024b; ORC, 2024a). Table 1 lists the standards from the OAC for the RN, and Table 2 lists the standards from the OAC for the LPN.
Table 1
OAC 4723-4-03: Standards Relating to Competent Practice as an RN
(A) A registered nurse shall provide nursing care within the scope of practice of nursing for a registered nurse as set forth in division (B) of section 4723.01 of the Revised Code and the rules of the board. (B) A registered nurse shall maintain current knowledge of the duties, responsibilities, and accountabilities for safe nursing practice. (C) A registered nurse shall demonstrate competence and accountability in all areas of practice in which the nurse is engaged including: (1) Consistent performance of all aspects of nursing care; and (2) Recognition, referral or consultation, and intervention, when a complication arises. (D) A registered nurse may provide nursing care that is beyond basic nursing preparation for a registered nurse, provided: (1) The nurse obtains education that emanates from a recognized body of knowledge relative to the nursing care to be provided; (2) The nurse demonstrates knowledge, skills, and abilities necessary to provide the nursing care; (3) The nurse maintains documentation satisfactory to the board of meeting the requirements set forth in paragraphs (D)(1) and (D)(2) of this rule; (4) When the nursing care is to be provided according to division (B)(5) of section 4723.01 of the Revised Code, the nurse has a specific current order from an individual who is authorized to practice in this state and is acting within the course of the individual's professional practice; and (5) The nursing care does not involve a function or procedure that is prohibited by any other law or rule. (E) A registered nurse shall, in a timely manner: (1) Implement any order for a patient unless the registered nurse believes or should have reason to believe the order is: (a) Inaccurate; (b) Not properly authorized; (c) Not current or valid; (d) Harmful, or potentially harmful to a patient; or (e) Contraindicated by other documented information; and (2) Clarify any order for a patient when the registered nurse believes or should have reason to believe the order is: (a) Inaccurate; (b) Not properly authorized; (c) Not current or valid; (d) Harmful, or potentially harmful to a patient; or (e) Contraindicated by other documented information. (F) When clarifying an order, the registered nurse shall, in a timely manner: (1) Consult with an appropriate licensed practitioner; (2) Notify the ordering practitioner when the registered nurse makes the decision not to follow the order or administer the medication or treatment as prescribed; (3) Document that the practitioner was notified of the decision not to follow the order or administer the medication or treatment, including the reason for not doing so; and (4) Take any other action needed to assure the safety of the patient. (G) A registered nurse shall, in a timely manner, report to and consult as necessary with other nurses or other members of the health care team and make referrals as necessary. (H) A registered nurse shall maintain the confidentiality of patient information. The registered nurse shall communicate patient information with other members of the health care team for health care purposes only, shall access patient information only for purposes of patient care, or for otherwise fulfilling the nurse's assigned job responsibilities, and shall not disseminate patient information for purposes other than patient care, or for otherwise fulfilling the nurse's assigned job responsibilities, through social media, texting, emailing, or any other form of communication. (I) To the maximum extent feasible, identifiable patient health care information shall not be disclosed by a registered nurse unless the patient has consented to the disclosure of identifiable patient health care information. A registered nurse shall report individually identifiable patient information without written consent in limited circumstances only and in accordance with an authorized law, rule, or other recognized legal authority. (J) The registered nurse shall use acceptable standards of safe nursing care as a basis for any observation, advice, instruction, teaching, or evaluation and shall communicate information which is consistent with acceptable standards of safe nursing care. (K) When a registered nurse provides direction to a licensed practical nurse the registered nurse shall first assess: (1) The condition of the patient who needs nursing care, including, but not limited to, the stability of the patient; (2) The type of nursing care the patient requires; (3) The complexity and frequency of the nursing care needed; (4) The training, skill, and ability of the licensed practical nurse who will be performing the specific function or procedure, to perform the specific function or procedure; and (5) The availability and accessibility of resources necessary to safely perform the specific function or procedure.
Effective: 2/1/2019 Last updated January 3, 2024 5-year Review Date: 10/2/2028 |
(OAC, 2024a)
Table 2
OAC 4723-4-04: Standards Relating to Competent Practice as an LPN
(A) A licensed practical nurse shall function within the scope of practice of nursing for a licensed practical nurse as set forth in division (F) of section 4723.01 of the Revised Code and the rules of the board. (B) A licensed practical nurse shall maintain current knowledge of the duties, responsibilities, and accountabilities for safe nursing practice. (C) A licensed practical nurse shall demonstrate competence and accountability in all areas of practice in which the nurse is engaged which includes, but is not limited to, the following: (1) Consistent performance of all aspects of nursing care; and (2) Recognition, referral or consultation, and intervention, when a complication arises. (D) A licensed practical nurse may provide nursing care in accordance with division (F) of section 4723.01 of the Revised Code that is beyond basic preparation for a licensed practical nurse provided: (1) The nurse obtains education that emanates from a recognized body of knowledge relative to the nursing care to be provided; (2) The nurse demonstrates knowledge, skills, and abilities necessary to perform the nursing care; (3) The nurse maintains documentation satisfactory to the board of meeting the requirements set forth in paragraphs (D)(1) and (D)(2) of this rule; (4) When the nursing care is to be provided according to division (F)(3) of section 4723.01 of the Revised Code, the nurse has a specific current valid order or direction from an individual who is authorized to practice in this state and is acting within the course of the individual's professional practice; and (5) The nursing care does not involve a function or procedure that is prohibited by any other law or rule. (E) A licensed practical nurse shall, in a timely manner: (1) Implement any order or direction for a patient unless the licensed practical nurse believes or should have reason to believe the order or direction is: (a) Inaccurate; (b) Not properly authorized; (c) Not current or valid; (d) Harmful, or potentially harmful to a patient; or (e) Contraindicated by other documented information; and (2) Clarify any order or direction for a patient when the licensed practical nurse believes or should have reason to believe the order or direction is: (a) Inaccurate; (b) Not properly authorized; (c) Not current or valid; (d) Harmful, or potentially harmful, to a patient; or (e) Contraindicated by other documented information. (F) When clarifying an order or direction, the licensed practical nurse shall, in a timely manner: (1) Consult with an appropriate licensed practitioner or directing registered nurse; (2) Notify the ordering practitioner or directing registered nurse when the licensed practical nurse makes the decision not to follow the order or direction or administer the medication or treatment as prescribed; (3) Document that the practitioner or directing registered nurse was notified of the decision not to follow the direction or order, or administer the medication or treatment, including the reason for not doing so; and (4) Take any other action needed to assure the safety of the patient. (G) A licensed practical nurse shall, in a timely manner, report to and consult as necessary with other nurses or other members of the health care team and make referrals as necessary. (H) A licensed practical nurse shall maintain the confidentiality of patient information obtained in the course of nursing practice. The licensed practical nurse shall communicate patient information with other members of the health care team for health care purposes only, shall access patient information only for purposes of patient care, or for otherwise fulfilling the nurse's assigned job responsibilities, and shall not disseminate patient information for purposes other than patient care, or for otherwise fulfilling the nurse's assigned job responsibilities, through social media, texting, emailing, or any other form of communication. (I) To the maximum extent feasible, identifiable patient health care information shall not be disclosed by a licensed practical nurse unless the patient has consented to the disclosure of identifiable patient health care information. A licensed practical nurse shall report individually identifiable patient information without written consent in limited circumstances only, and in accordance with an authorized law, rule, or other recognized legal authority. (J) When a licensed practical nurse is directed to observe, advise, instruct, or evaluate the performance of a nursing task, the licensed practical nurse shall use acceptable standards of safe nursing care as a basis for that observation, advice, instruction, teaching, or evaluation and shall communicate information that is consistent with acceptable standards of safe nursing care.
Effective: 2/1/2019 Last updated 01/03/2024 5-Year Review Date: 10/2/2028 |
(OAC, 2024b)
Specific areas addressed in the OAC include maintaining and demonstrating competency; assuring patient safety; maintaining confidentiality; delineating, establishing, and maintaining professional boundaries; and applying the nursing process (OAC, 2024a, 2024b).
- The rules related to competency are found in 4723-4-03 (A)-(G) for RNs (refer to Table 1) and 4723-4-04 (A)-(G) for LPNs (refer to Table 2). Both LPNs and RNs are accountable for maintaining current knowledge and demonstrating competency and consistent nursing care performance. When providing care beyond basic nursing preparations, the nurse must maintain documentation to demonstrate that they obtained advanced knowledge from a credible source (OAC, 2024a, 2024b).
- The OBN expects nurses to implement orders from licensed providers in a timely manner unless there is a reason to believe that the order is inappropriate for the patient. Additional details about this can be found in 4723-4-03 (E; refer to Table 1) and 4723-4-04 (E; refer to Table 2). The OBN expects the nurse to report to and consult with other nurses and health care team members and to make necessary referrals. This information is detailed in 4723-4-03 (G; refer to Table 1) and 4723-4-04 (G; refer to Table 2). 4723-4-03 (J; see Table 1) and 4723-4-04 (J; refer to Table 2) outline the OBN's regulations regarding acceptable standards of safe nursing care as a basis for providing advice, instruction, teaching, and evaluation of nursing care (OAC, 2024a, 2024b).
- The regulations related to confidentiality are found in 4723-4-03 (H; refer to Table 1) and 4723-4-04 (H; refer to Table 2). The OBN requires the nurse to carefully safeguard patient information and only access and disseminate information to provide patient care or fulfill job responsibilities (OAC, 2024a, 2024b).
- The regulations related to professional boundaries and misappropriation of property are found in 4723-4-06 (H), (I), (J), (K), (L), and (M). The OBN requires the nurse to provide privacy during examination, treatment, and when providing personal care. In addition, the OBN requires the nurse to demonstrate courtesy and respect each patient's individuality (OAC, 2024d).
Section 4723-4-05 of the OAC outlines the standards of care for APRNs. These standards are generalized and apply to CNMs, CNPs, CRNAs, and CNS advanced practice providers (OAC, 2024c). Table 3 outlines Rule 4723-4-05.
Table 3
OAC 4723-4-05: Standards Relating to Competent Practice as an APRN
(A) A certified nurse-midwife, certified nurse practitioner, certified registered nurse anesthetist, or clinical nurse specialist shall do all of the following: (1) Function within the scope of practice of nursing for a registered nurse as set forth in division (B) of section 4723.01 of the Revised Code and the rules of the board. (2) Function within the nurse's applicable scope of practice as set forth in section 4723.43 of the Revised Code and the rules of the board. (3) If authorized by Ohio law to prescribe, practice according to section 4723.481 of the Revised Code and Chapter 4723-9 of the Administrative Code. (B) When the practice of a certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist is evaluated, the evaluation shall be provided by a collaborating licensed physician or podiatrist, or an advanced practice registered nurse holding a current, valid license with the same designation as the individual being evaluated. (C) When the practice of a certified registered nurse anesthetist is evaluated, the evaluation shall be provided by a supervising licensed physician, podiatrist, dentist or a certified registered nurse anesthetist whose license is current and valid. (D) A certified nurse-midwife, certified nurse practitioner, certified registered nurse anesthetist, or clinical nurse specialist may provide care within their specialty provided: (1) The nurse obtains education that emanates from a recognized body of knowledge relative to the nursing care to be provided; (2) The nurse demonstrates knowledge, skills, and abilities necessary to provide the nursing care; and (3) The nurse maintains documentation satisfactory to the board of meeting the requirements set forth in paragraphs (D)(1) and (D)(2) of this rule. Effective: 2/1/2019 Last updated 1/3/2024 5-Year Review Date: 10/2/2028 |
(OAC, 2024c)
To practice in Ohio, the APRN must enter into a standard care agreement with at least one physician or podiatrist. The exception is that any certified psychiatric-mental health CNS or psychiatric-mental health NP cannot enter into a collaborative agreement with a podiatrist (OAC, 2022b). Standard care arrangements are addressed in rule 4723-8-04 of the OAC, as outlined in Table 4.
Table 4
OAC 4723-8-04: Standard Care Arrangement for a CNM, CNP, or CNS
(A) Prior to engaging in practice, a standard care arrangement shall be entered into with each physician or podiatrist with whom the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist collaborates. (1) The standard care arrangement shall be revised to reflect the addition or deletion of a physician or podiatrist with whom the nurse collaborates within that employment setting. Under these circumstances, a new standard care arrangement is not necessary. (2) A new standard care arrangement shall be executed when the nurse is: (a) Employed at a different or additional organization or practice; and (b) Engages in practice with a collaborating physician or podiatrist outside of the primary employing organization. (B) Except as provided in paragraph (C) of this rule, a certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist engaged in the practice of the nurse's specialty, shall enter into a written standard care arrangement with one or more collaborating physicians or podiatrists whose practice is the same or similar to the nurse's practice. (C) In accordance with division (A)(2)(c) of section 4723.431 of the Revised Code, a clinical nurse specialist certified as a psychiatric-mental health CNS by the American nurses credentialing center or a certified nurse practitioner who is certified as a psychiatric-mental health NP by the American nurses credentialing center, may enter into a standard care arrangement with a physician, but not a podiatrist, if the collaborating physician is practicing in one of the following specialties: (1) Psychiatry; (2) Pediatrics; (3) Primary care of family practice. (D) The standard care arrangement shall include at least: (1) The signatures of each nurse, and each collaborating physician, or the physician's designated representative, or each podiatrist with whom the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist primarily collaborates indicating review of and agreement to abide by the terms of the standard care arrangement. For purposes of this rule, a physician's designated representative means a physician who serves as the department or unit director or chair, within the same institution, organization or facility department or unit, and within the same practice specialty, that the nurse practices, and with respect to whom the physician has executed a legal authorization to enter collaborating agreements on the physician's behalf; (2) The date when the arrangement is initially executed; (3) The date of the most recent review of the arrangement; (4) The complete name, specialty and practice area, business address, and business phone number or number at which the individual can be reached at any time for: (a) Each collaborating physician or podiatrist with whom the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist primarily collaborates and who is a party to the standard care arrangement, unless a physician's designated representative has entered the standard care arrangement on the physician's behalf; and (b) Each certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist who is a party to the standard care arrangement; (5) A statement of services offered by the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist consistent with section 4723.43 of the Revised Code and this chapter, including a description of the scope of prescriptive practice and authorization to enter consult agreements for patients, if applicable; (6) A plan for incorporation of new technology or procedures consistent with the applicable scope of practice as set forth in section 4723.43 of the Revised Code and this chapter; (7) Quality assurance provisions, including at least: (a) When modification is made to the body of the standard care arrangement, reapproval of the standard care arrangement is required; (b) Criteria for referral of a patient by the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist to a collaborating physician or podiatrist, including, for the certified nurse-midwife, a plan for referral of breech or face presentation or any other abnormal condition identified as such in the standard care arrangement; (c) A process for the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist to obtain consultation from a physician or podiatrist; and (d) A process for chart review in accordance with rule 4723-8-05 of the Administrative Code if the nurse's practice includes any direct patient care; (8) A plan for coverage of patients in instances of emergency or planned absences of either the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist, or the collaborating physician or podiatrist; (9) A process for resolution of disagreements regarding matters of patient management; and (10) Regarding the prescribing component of the clinical nurse specialist, certified nurse-midwife, or certified nurse practitioner's practice, the following quality assurance provisions shall include at least: (a) Provisions to ensure timely direct, personal evaluation of the patient with a collaborating physician or the physician's designee when indicated; (b) Prescribing parameters for drugs or therapeutic devices when indicated; (c) Provisions for the use of schedule II controlled substances; (d) If the nurse is prescribing to minors, as defined in division (A) of section 3719.061 of the Revised Code, provisions for complying with section 3719.061 of the Revised Code when prescribing an opioid analgesic to a minor; and (e) Provisions for obtaining and reviewing OARRS reports, and engaging in physician consultation and patient care consistent with section 4723.487 of the Revised Code and rule 4723-9-12 of the Administrative Code. (11) Quality assurance standards consistent with rule 4723-8-05 of the Administrative Code. (E) The most current copy of the standard care arrangement, and any legal authorization signed by a physician according to paragraph (D)(1) of this rule, shall be retained on file by the nurse's employer. Upon request of the board, the certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist shall immediately provide a copy of the standard care arrangement to the board. (F) Copies of previously effective standard care arrangements shall be retained by the nurse for three years and provided to the board upon request. (G) When a hospital negotiates a standard care arrangement in accordance with division (E) of section 4723.431 of the Revised Code and this chapter, the standard care arrangement shall be developed in accordance with paragraph (D) of this rule. Review and approval of the standard care arrangement shall be in accordance with the policies and procedures of the hospital governing body and the bylaws, policies, and procedures of the hospital medical staff. (H) A certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist shall notify the board of the identity of a collaborating physician or podiatrist not later than thirty days after engaging in practice. (I) A certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist shall notify the board of any change in the name and business address of a collaborating physician or podiatrist not later than thirty days after the change takes effect, except as provided in division (D) of section 4723.431 of the Revised Code.
Effective and last updated: 2/1/2022 5-year Review Date: 10/15/2025 |
(OAC, 2022b)
The prescriptive authority of APRNs is addressed in Section 4723.481 of the ORC (2024d) and Section 4723-9 of the OAC (2022c). This section of the ORC sets the standards related to the prescriptive authority of APRNs and specifies that APRNs are only permitted to prescribe medications or medical devices not appearing on the exclusionary formulary listed under section 4723.5 of the ORC (i.e., any drug to induce abortion). The prescriptive capability of the APRN cannot exceed that of their collaborating physician or podiatrist. APRNs can only prescribe schedule II narcotics when specific criteria are met. There are exceptions for APRNs practicing in particular settings, such as long-term care facilities, birthing centers, hospitals, or ambulatory surgical centers (OAC, 2022c). The schedule II criteria that must be met include the following:
- The patient must have a terminal condition.
- The quantity must be limited to a 3-day supply.
- The medication was initially prescribed by a physician (ORC, 2024d).
Evaluations of an APRN must be completed by a collaborating physician, dentist, podiatrist, or registered anesthetist with a current and valid license with the same designation as the APRN being evaluated (OAC, 2024c). The APRN can provide care within their specialty provided they:
- Demonstrate the knowledge, skills, and abilities of the specialty.
- Obtain appropriate education from a recognized body of knowledge.
- Document evidence of skills and abilities, and maintain records as required (OAC, 2024c).
Refer to Table 5 for the standards of care for the APRN outlined in rule 4723-8-02 of the OAC.
Table 5
OAC 4723-8-02: APRN Certification and Practice: Standards of Practice
(A) An advanced practice registered nurse shall provide to patients nursing care that requires knowledge and skill obtained from advanced formal education, which includes a clinical practicum, and clinical experience as specified in sections 4723.41, 4723.43, 4723.433, 4723.434, 4723.435 and 4723.482 of the Revised Code and this chapter. (B) Except as otherwise precluded by law or rule, each advanced practice registered nurse shall practice in accordance with the following: (1) The advanced practice registered nurse's education and clinical experience; (2) The advanced practice registered nurse's national certification as provided in section 4723.41 of the Revised Code; and (3) Chapter 4723. of the Revised Code and rules adopted under that chapter. (C) Only a certified nurse-midwife, certified nurse practitioner, or clinical nurse specialist holding a current valid license as an advanced practice registered nurse may prescribe drugs. A certified registered nurse anesthetist may order drugs for use in the health care facility where the nurse practices in accordance with sections 4723.434 and 4723.435 of the Revised Code. (D) Each certified nurse-midwife, certified nurse practitioner, and clinical nurse specialist shall utilize and incorporate into the nurse's practice, knowledge of Chapter 4731. of the Revised Code and rules adopted under that chapter that govern the practice of the nurse's collaborating physician or podiatrist. Each certified registered nurse anesthetist shall utilize and incorporate into the nurse's practice, knowledge of Chapters 4715. and 4731. of the Revised Code and rules adopted under these chapters that govern the practice of the nurse's supervising podiatrist, dentist, or physician. (E) Nothing in this rule precludes an advanced practice registered nurse from practicing as a registered nurse in accordance with section 4723.01 of the Revised Code and the rules of the board.
Effective: 2/1/2021 5-year Review Date: 10/15/2025 |
(OAC, 2021a)
Another aspect of the OAC for APRNs is title protection, which prohibits nurses from using an inappropriate or unearned credential when functioning as a licensed APRN. Only those with a valid license to practice as an APRN and have met all the criteria outlined in ORC 4723.41, 4723.42, and 4723.482 can utilize the specific APRN credentials associated with their role and specialty (i.e., CNP, CNM, CRNA, CNS). Additional information on title protection for the APRN can be found within OAC 4723-8-03 (OAC, 2021b).
| Further information related to the APRN role can be found throughout OAC 4723-8. |
Scope of Practice
All nurses must provide care within their scope of practice, and the nursing care provided should be aligned with the individual nurse's education, knowledge, experience, and demonstrated competency. Since nursing is a dynamic practice, questions about the nurse's scope of practice may arise. To assist in delineating the scope of practice, the OBN developed a Scope of Practice Decision-Making Model (refer to Figure 1). The model incorporates a decision tree that includes references and is based on safety, competency, legality, and accountability (OBN, 2019).
Figure 1
OBN RN and LPN Decision-Making Model
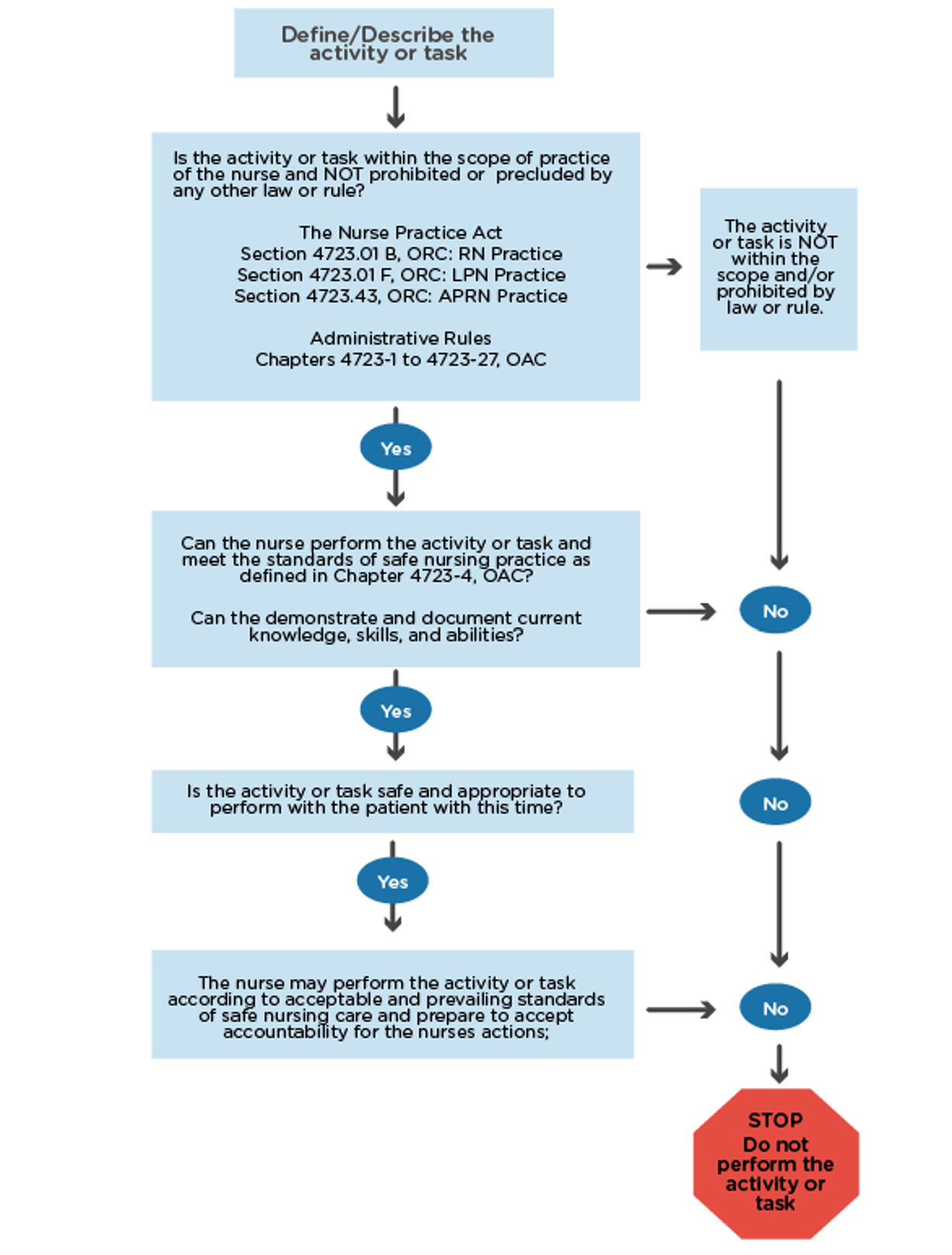
(OBN, 2019)
Promoting Patient Safety
As discussed before, the BON's role is to protect the public from the unsafe delivery of nursing care. The standards of nursing practice that promote patient safety are outlined in rule 4723-4-06 of the OAC (2024d). To protect the patient, the OAC prohibits engaging in:
- Behavior that may be viewed as abuse or that results in physical, mental, or emotional harm to a patient.
- Actions that might reasonably be interpreted as verbally, physically, mentally, or emotionally abusive.
- Misappropriation of a patient's personal property.
- Attempts to seek personal benefit at the expense of the patient.
- Activities that can be reasonably interpreted as inappropriate involvement in the patient's personal relationships or financial behaviors.
- Sexual activities or conduct with a patient.
- Conduct or verbal exchanges while delivering care that might reasonably be construed as sexual, seductive, or demeaning to the patient (OAC, 2024d).
The OAC establishes standards for applying the nursing process as an RN. These regulations can be found in OAC 4723-4-07 and are outlined as follows (OAC, 2024e).
- RNs must use the steps of the nursing process (assessment, analysis, planning, implementation, and evaluation) in nursing practice.
- Effective use of the nursing process requires nurses recognize its dynamic nature and, thus, respond to changes in the patient's health status.
- The RN should begin with assessing the patient's status (collecting objective and subjective data from the patient, family, and other sources).
- The RN then documents findings, analyzes and reports those findings, develops and modifies the plan of care as needed, and communicates the plan of care to other members of the health care team.
- The RN implements the plan of care by carrying out the nursing regimen.
- The RN provides care that is within their scope of practice.
- The RN collaborates with and provides assistance to other health care team members.
- Finally, the RN evaluates the patient's response to determine the effectiveness of the treatment and care plan. The nurse might need to revise the plan of care based on the evaluation. The nurse may also need to notify the provider if an adjustment in the patient's care plan is warranted based on the evaluation findings.
The standards for applying the nursing process are slightly different as an LPN. According to OAC 4723-4-08, LPNs must contribute to the nursing process by providing care based on the established nursing plan. LPNs also use data collection, planning, implementation, and evaluation as described in the bullet points above in their nursing practice (OAC, 2023b).
Disciplinary Process
According to the NCSBN (n.d.-b), most licensed nurses in the US provide safe, competent, and compassionate nursing care. In addition, less than 1% of nurses are disciplined by their respective BON. Likewise, the OBN reports that most Ohio nurses practice with high standards. However, when a nurse allegedly violates OBN's laws or rules, they are subject to disciplinary action (NCSBN, n.d.-b; OAC, 2024g).
In carrying out its disciplinary responsibilities, the OBN has the authority to revoke or suspend any license or certificate endorsed by the board; impose probationary requirements, reprimands, fines, or practice restrictions; and deny initial or renewal licenses or certifications. The disciplinary process typically begins when a patient, family member, nurse manager, or employer files a complaint. Refer to Table 6 for detailed information about the number of complaints and a partial list of the types of complaints the OBN received during fiscal years 2020 to 2024. This information is publicly available and is posted on the OBN website within the Annual Report. Please note that 2021 OBN disciplinary data was not available for review and therefore is not displayed. Additionally, some disciplinary categories were changed in 2024, making the categories of “multiple allegations” and “noncompliance with board action” not applicable (OBN, n.d.-c).
Table 6
OBN Disciplinary Data
Year | 2020 | 2022 | 2023 | 2024 |
Number of complaints | 6,540 | 6,053 | 6,906 | 7,183 |
Confidentiality | 45 | 57 | 57 | 72 |
Criminal | 391 | 366 | 336 | 429 |
Drugs/alcohol | 556 | 543 | 561 | 553 |
Fraud | 48 | 43 | 26 | 19 |
Multiple allegations | 67 | 82 | 108 | N/A |
Noncompliance with board action | 443 | 236 | 203 | N/A |
Patient abuse | 53 | 50 | 51 | 56 |
Practice | 1,025 | 739 | 971 | 743 |
(OBN, n.d.-c)
The OBN is the governing body within the state that upholds the NPA and the rules found in the OAC. The NPA lays out the process by which the OBN investigates evidence when it appears that a nurse has failed to practice in accordance with acceptable standards of safe practice. After the evidence has been gathered, a thorough review by the OBN is performed to determine the presence of wrongdoing or of a deficiency in practice without harm or risk of serious imminent harm (indicating that the NPA may offer a less stringent alternative). ORC section 4723.28, related to disciplinary action for nurses, was updated as of March 21, 2025. This update reflects the addition of (38) Violation of section 4723.93 of the Revised Code. (Consent for Intimate examination; ORC, 2024b).
| Additional information on disciplinary actions for nurses can be found within the Ohio Revised Code-ORC 4723.28. |
License Renewal and Education Requirements
Most states require evidence of continued professional development as part of the license renewal process for nurses to continue to practice. For nurses in Ohio, the renewal cycle is every 2 years from November 1 to October 31 (on even years for LPNs and odd years for RNs). During each licensure cycle, the nurse is required to complete and maintain records for 24 contact hours of continuing education (CE) approved by the OBN. One hour of these 24 hours must be regarding category A training, and up to 8 hours can be satisfied by providing volunteer health care services. Those who have held a nursing license by endorsement in Ohio for 1 year or less at the time of renewal are only required to obtain 12 CE hours. A nurse who gains licensure through examination is exempt from the CE requirements for the first renewal cycle following examination (OAC, 2022a, 2023d).
Each nurse applying for renewal is required to attest to having completed the required 24 contact hours at an appropriate level within the 2-year timeframe. Documentation must be provided within 60 days if requested by the OBN during routine audits. If evidence is not provided or the individual does not meet the requirements upon request, their license will be inactivated, and they are not eligible for renewal, reactivation, or reinstatement until the continuing education requirements are met. To reactivate or reinstate a lapsed license, the nurse applicant must complete 24 contact hours of CE. Of these, at least 1 hour must pertain to category A, and the applicant must maintain documentation that the hours were completed during the 24 months before their reapplication date. The OBN allows for one waiver period per license. A waiver request must be submitted to the OBN and cannot be withdrawn once requested. The waiver eliminates the CE requirements for one renewal cycle (OAC, 2023d).
Specific initial licensure and renewal requirements for LPNs, RNs, and APRNs can be found on the OBN website and within OAC 4723-14-03. The current CE requirements for license renewal for LPNs/RNs are listed in Table 7.
Table 7
OAC 4723-14-03 (A-D): Continuing Education Requirements for LPNs and RNs
(A) A nurse applying to renew an active license to practice nursing as a licensed practical nurse or registered nurse in Ohio must complete twenty-four contact hours of continuing education during the renewal period, unless an exception applies, and at least one of the required hours needs to be in category A continuing education. (1) For the period immediately following licensure by examination, a nurse who holds an active license to practice nursing in Ohio is not required to complete any contact hours of continuing education for the first license renewal; (2) A nurse who has been licensed by endorsement in Ohio for one year or less must complete twelve contact hours of continuing education; (3) A nurse who has been licensed by endorsement in Ohio for more than one year must complete twenty-four contact hours of continuing education. (B) A licensed practical nurse who has an active license as a registered nurse in Ohio is not required to meet the continuing education requirement for renewal of the license to practice as a practical nurse. (C) A nurse from another jurisdiction who applies for licensure by endorsement to practice as a licensed practical nurse or registered nurse in Ohio is required to complete two contact hours of category A continuing education in order to be eligible for licensure. (D) In order to renew, applicants must attest to completion of the continuing education required by this rule on the application for renewal. The board may require a renewal applicant to show proof of completion of continuing education. If the board requests proof of continuing education and the applicant fails to provide proof to the board before the end of the renewal period, the license shall lapse. *"Category A" means the portion of CE that meets the 1 hour requirement directly related to Chapter 4723 of the Revised Code and the rules of the board as described In rule 4723-14-03 of the Administrative Code. To qualify as category A, the CE must be approved by the board, an OBN approver, or offered by an approved provider unit headquartered In the state of Ohio. 4723-14-01(E) (OAC, 2024f). |
(OAC, 2023d)
Education activities for CE should be approved by an OBN approver or administered by an approved provider unit as listed by the OBN, which includes those accredited by the American Nurses Credentialing Center (ANCC), the Accreditation Council for Continuing Medical Education (ACCME), or the International Association for Continuing Education and Training (IACET). Academic credit taken through an accredited educational institution can also be utilized towards a nurse's CE requirements, along with an independent study or volunteer hours spent caring for indigent or uninsured populations. As with RNs, APRNs in Ohio are not required to submit proof of CE hours obtained during their first licensure renewal after initial licensure by examination. CE hours for all other renewing APRNs in Ohio must be obtained between November 1 and October 31 of odd-numbered years. APRNs are required to complete 24 contact hours of CE in the 24-month renewal cycle, including 12 hours of advanced pharmacology training if they are active prescribers in addition to the 24 hours of CE they are required to obtain for the RN licensure renewal. This requires a total of 48 contact hours for the 2-year renewal period. These hours may also be used towards their national certification (OBN, n.d.-a; ORC, 2017b).
Delegation of Tasks and Supervision
The nursing world functions as a multidisciplinary and cohesive team with care provided by various professionals at different licensure levels and corresponding scopes of practice. The APRN can delegate tasks to RNs, LPNs, and unlicensed assistive personnel (UAP) within this structure. For more information on some portions of APRN delegation, refer to the ORC 4723.48 (ORC, 2023b). RNs can delegate tasks to LPNs and UAPs. LPNs can delegate tasks to UAP. In Ohio, an LPN may only delegate to a UAP under the RN's direction (OAC, 2023c). The delegation of medication administration to medication aides in Ohio is covered in ORC 4723.67, which has a new version that took effect March 20, 2025 (ORC, 2024c). This delegation must be done within the scope of practice. Assigning, delegating, and supervising are skills that nurses may need to use in order to manage the needs of their assigned patients. To utilize these skills, the nurse must understand the difference between the following terms (ANA, 2023).
- Assigning refers to transferring authority, accountability, and responsibility of patient care to another health care team member.
- Delegating refers to transferring the authority and responsibility of a task to another health care team member, while retaining accountability.
- Supervising refers to directing, monitoring, and evaluating the performance of tasks completed by another health care team member. RNs are responsible for supervising tasks delegated to an LPN or UAP.
Nurses must assign, delegate, and supervise appropriately, following the ANA professional standards, health care facility policies, and state NPA. Assigning occurs in a downward or lateral manner to another health care team member (ANA, 2023). The OAC defines “direction” as “communicating a plan of care to an LPN. Direction by an RN is not meant to imply the RN is supervising the LPN in the employment context” (OAC, 2024f).
When assigning, the nurse should consider various factors, including:
- Condition of the patient and level of care
- Need for specific precautions (i.e., seizure, fall, isolation)
- Particular care needs (i.e., cardiac monitoring, wound care)
- Knowledge and skill of the team member
- Staffing mix (i.e., RN, LPN, UAP)
- Nurse-to-patient ratio
- Experience of staff with similar patients
- Amount of supervision required (ANA & NCSBN, 2019)
The delegating nurse must consider the following.
- Task factors
- Potential for harm (i.e., bleeding, aspiration, fall)
- Predictability of outcome (i.e., is it a routine treatment with a predictable outcome)
- Need for problem-solving and innovation (i.e., clinical judgment or assessment)
- Complexity of care (i.e., is the delegatee qualified to perform the skill)
- Level of interaction with the patient (i.e., is education required)
- Delegatee factors
- Knowledge, training, and experience
- Demonstrated competence
- Institutional policies and licensing legislation
- Ability to communicate with others
- Five rights of delegation
- Right task (i.e., the task should be appropriate and require minimal supervision and risk of harm)
- Right circumstance (i.e., assess the complexity of care and match this to the skill level of the delegatee)
- Right person (i.e., assess and verify the delegatee's scope of practice, training, and competence)
- Right direction/communication
- Data to be collected
- Specific task to be performed
- Method and timeline for reporting concerns or findings
- Expected results
- Right supervision/evaluation
- Provide supervision directly or indirectly (i.e., assign to another licensed nurse)
- Monitor performance
- Provide feedback
- Evaluate the patient and determine if outcomes were met
- Intervene if necessary (i.e., unsafe practices) (ANA, 2023; ANA & NCSBN, 2019)
Table 8
Tasks Appropriate for Delegation from an RN to an LPN or UAP
LPN | UAP |
|
|
(Nursing OnPoint, 2022; OAC, 2023b, 2023c; ORC, 2023a)
The OAC defines safe delegation within nursing in rule 4723-13 (2023c) and specifies that only a licensed nurse may delegate a task to an unlicensed person. Once a nursing task has been delegated, it cannot be delegated (passed along) to another individual. In Ohio, a licensed nurse may delegate the administration of an over-the-counter topical medication to improve a skin condition or provide a barrier or an over-the-counter eye/ear drop or suppository. They may also delegate foot soak treatments and enemas to UAPs if appropriate. Delegated tasks must be within the licensed nurse’s scope of practice, knowledge, skill, and ability. The task must be within the delegatee's training, ability, and skill. The required resources/support to complete the task are evident, including the supervision by the licensed nurse. Tasks that require judgment based on nursing knowledge, complex observations, critical decision-making, and nursing assessment or that may have unpredictable outcomes are not appropriate to delegate to UAPs. Delegated tasks should be able to be completed using specific, consistent directions without alteration. Tasks should have minimal repercussions if performed incorrectly. Ultimately, the delegating licensed nurse is held accountable for their decision to delegate with the ability (and intention) to intervene if the task is being performed incorrectly. When teaching a UAP to perform a task, the nurse should provide background information, including the concepts underlying the task, infection control and universal precautions, and step-by-step instructions. The licensed nurse should demonstrate the task and then observe and document a return demonstration by the UAP. OAC rule 4723-13-07 (A) states that supervision should be onsite when providing health care services and may include “initial and ongoing direction, procedural guidance, and evaluation, and may include direct observation of the performance of the nursing task” (OAC, 2023c).
Important Note and Disclaimer
The information in this module is general in nature and is not, nor intended to be, legal advice. The laws are complex, and circumstances vary. Therefore, you should consult an attorney for advice regarding your individual situation.
References
American Nurses Association. (2023). Delegation in nursing: How to build a stronger team. https://www.nursingworld.org/content-hub/resources/nursing-leadership/delegation-in-nursing/
American Nurses Association and the National Council of State Boards of Nursing. (2019). National guidelines for nursing delegation. https://www.nursingworld.org/globalassets/practiceandpolicy/nursing-excellence/ana-position-statements/nursing-practice/ana-ncsbn-joint-statement-on-delegation.pdf
Graduatenursing.edu. (n.d.). What is a state board of nursing? Retrieved February 10, 2025, from https://www.graduatenursingedu.org/state-board-of-nursing
National Council of State Boards of Nursing. (n.d.-a). About U.S. nursing regulatory bodies. Retrieved February 10, 2025, from https://www.ncsbn.org/nursing-regulation/about-nursing-regulatory-bodies.page
National Council on State Boards of Nursing. (n.d.-b). Discipline. Retrieved February 10, 2025, from https://www.ncsbn.org/nursing-regulation/discipline.page
Nursing OnPoint. (2022). Delegation & scope of practice for nurses. https://nursingonpoint.com/education/nursing-degrees-guides-to-practice/delegation-scope-of-practice-worksheet/
Ohio Administrative Code. (2021a). Rule 4723-8-02: Standards of practice. https://codes.ohio.gov/ohio-administrative-code/rule-4723-8-02
Ohio Administrative Code. (2021b). Rule 4723-8-03: Title protection. https://codes.ohio.gov/ohio-administrative-code/rule-4723-8-03
Ohio Administrative Code. (2022a). Rule 4723-7-09: License renewal for licensed practical nurses and registered nurses. https://codes.ohio.gov/ohio-administrative-code/rule-4723-7-09
Ohio Administrative Code. (2022b). Rule 4723-8-04: Standard care arrangement for a certified nurse-midwife, certified nurse practitioner, and clinical nurse specialist. https://codes.ohio.gov/ohio-administrative-code/rule-4723-8-04
Ohio Administrative Code. (2022c). Rule 4723-9-10: Formulary; standards of prescribing for advanced practice registered nurses designated as clinical nurse specialists, certified nurse-midwives, or certified nurse practitioners. https://codes.ohio.gov/ohio-administrative-code/rule-4723-9-10
Ohio Administrative Code. (2023a). Rule 4723-1-01: Board organization. https://codes.ohio.gov/ohio-administrative-code/rule-4723-1-01
Ohio Administrative Code. (2023b). Rule 4723-4-08: Standards for applying the nursing process as a licensed practical nurse. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-08
Ohio Administrative Code. (2023c). Rule 4723-13: Delegation of nursing tasks. https://codes.ohio.gov/ohio-administrative-code/chapter-4723-13
Ohio Administrative Code. (2023d). Rule 4723-14-03: Continuing education requirement for licensed practical and registered nurses. https://codes.ohio.gov/ohio-administrative-code/rule-4723-14-03
Ohio Administrative Code. (2024a). Rule 4723-4-03: Standards relating to competent practice as a registered nurse. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-03
Ohio Administrative Code. (2024b). Rule 4723-4-04: Standards relating to competent practice as a licensed practical nurse. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-04
Ohio Administrative Code. (2024c). Rule 4723-4-05: Standards relating to competent practice as a certified nurse-midwife, certified nurse practitioner, certified registered nurse anesthetist, or clinical nurse specialist. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-05
Ohio Administrative Code. (2024d). Rule 4723-4-06: Standards of nursing practice promoting patient safety. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-06
Ohio Administrative Code. (2024e). Rule 4723-4-07: Standards for applying the nursing process as a registered nurse. https://codes.ohio.gov/ohio-administrative-code/rule-4723-4-07
Ohio Administrative Code. (2024f). Rule 4723-14-01: Definitions. https://codes.ohio.gov/ohio-administrative-code/rule-4723-14-01
Ohio Administrative Code. (2024g). Rule 4723-16-07: Evidence or factors to be considered by the board. https://codes.ohio.gov/ohio-administrative-code/rule-4723-16-07
The Ohio Board of Nursing. (n.d.-a). CE requirements for license renewal. Retrieved February 10, 2025, from https://nursing.ohio.gov/continuing-education-and-pre-licensure/continuing-education/ce-requirements-for-renewal
The Ohio Board of Nursing. (n.d.-b). About us: Ohio Board of Nursing. Retrieved February 12, 2025, from https://nursing.ohio.gov/about-us/ohio-board-of-nursing
The Ohio Board of Nursing. (n.d.-c). OBN annual & fiscal reports. Retrieved February 10, 2025, from https://nursing.ohio.gov/about-us/boards-reports/fiscal-annual-reports
The Ohio Board of Nursing. (2019). RN and LPN decision-making model. https://nursing.ohio.gov/wps/wcm/connect/gov/3642faaa-ea51-4562-bd9b-68f73c7ec1cc/decision-making-model20191007_14055357.pdf
The Ohio Legislature 136th General Assembly. (n.d.). Laws. Retrieved February 10, 2025, from https://www.legislature.ohio.gov/laws
Ohio Revised Code. (2017a). Section 4723.02: Board of Nursing. https://codes.ohio.gov/ohio-revised-code/section-4723.02
Ohio Revised Code. (2017b). Section 4723.24: License or certification renewal; notice of change of address. https://codes.ohio.gov/ohio-revised-code/section-4723.24
Ohio Revised Code. (2023a). Section 4723.01: Nurse definitions. https://codes.ohio.gov/ohio-revised-code/section-4723.01
Ohio Revised Code. (2023b). Section 4723.48: Delegation of authority to administer certain drugs. https://codes.ohio.gov/ohio-revised-code/section-4723.48
Ohio Revised Code. (2024a). Section 4723.06: Board of nursing – powers and duties. https://codes.ohio.gov/ohio-revised-code/section-4723.06
Ohio Revised Code. (2024b). Section 4723.28: Disciplinary actions. http://codes.ohio.gov/orc/4723.28
Ohio Revised Code. (2024c). Section 4723.67: Administration of medication by aides- delegation by nurse required. https://codes.ohio.gov/ohio-revised-code/section-4723.67
Ohio Revised Code. (2024d). Section 4723.481: Authority of A.P.R.N. designated as clinical nurse specialist, certified nurse-midwife, or certified nurse practitioner to prescribe drugs and therapeutic devices. https://codes.ohio.gov/ohio-revised-code/section-4723.481
Powered by Froala Editor