About this course:
This course reviews the pathophysiology, risk factors, clinical manifestations, diagnosis, and management of patients with an acute stroke within the brain.
Course preview
Acute Stroke for RNs and LPNs
Upon completion of this module, learners should be able to:
- explore vital statistics regarding stroke in the US and worldwide
- review the basics of cerebral vascular anatomy
- describe the pathophysiology involved in both ischemic and hemorrhagic strokes
- discuss the risk factors and prevention strategies for stroke
- identify the signs and symptoms of a stroke
- describe the components of a full stroke workup and acute treatment options, including surgical treatment for hemorrhagic strokes, thrombolytics, and endovascular procedures
- discuss the rehabilitation process following a stroke
Cardiovascular disease (CVD) is the leading cause of death globally. In 2019, 32% of all global deaths, or an estimated 17.9 million people, died from CVDs, with 85% due to a heart attack or stroke. Over 75% of these deaths occurred in middle-to-low-income countries (World Health Organization [WHO], 2021). Within the US adult population, roughly 9.4 million people ages 20 and older self-report having had a stroke, equating to an overall prevalence of 3.3%. Each year around 795,000 people in the US have a stroke, with 610,000 being first-time strokes and 185,000 being recurrent. Approximately 85% of all strokes are ischemic. Stroke is the fifth leading cause of death in the US, but the risk varies with race and ethnicity. Non-Hispanic Black adults are twice as likely to have a stroke than White adults. In addition, non-Hispanic Black adults and Pacific Islander adults have the highest mortality rates due to stroke. Women are also more likely to die secondary to stroke than men. Approximately 160,264 people in the US die annually following a stroke, with 69,637 deaths occurring in males and 90,627 in females. Even with enhanced primary prevention practices and technology to treat patients diagnosed with a stroke, it is estimated that by 2030, an additional 3.4 million adults in the US (3.9%) will have a stroke, a 20.5% increase since 2012. The largest increase is projected in White Hispanic males (29%). The estimated cost of stroke-related care in the US is $56.5 billion annually, including healthcare services, medications, and lost productivity. There is a significant variation in mortality regionally across the US, with a much higher mortality rate seen in the "stroke belt" of the southeast (North and South Carolina, Georgia, Tennessee, Mississippi, Alabama, Louisiana, and Arkansas; Centers for Disease Control and Prevention [CDC], 2023b; Tsao et al., 2023; Winstein et al., 2016). See Figure 1 for mortality rates from stroke nationwide.
Figure 1
Stroke Death Rate per 1000,000 from 2018-2020
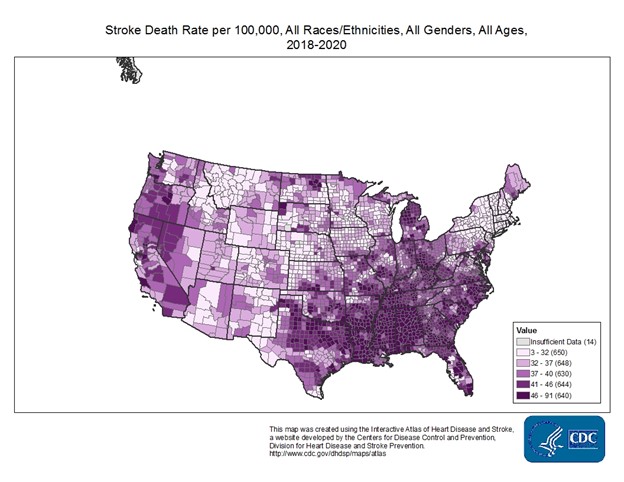
(CDC, n.d.)
Pathophysiology
The anatomy of cerebral circulation starts with the common carotid arteries (Figure 2), which split into the external and internal carotid arteries (ICAs). The external carotid arteries supply the posterior scalp and face. The ICAs supply blood to roughly 80% of the cerebrum. From there, the anterior cerebral artery branches off to supply the superior portion of the frontal and parietal lobes. The ophthalmic and middle cerebral arteries (MCA) also branch off the ICAs. The ophthalmic artery supplies the ocular orbit and some structures in the nose, face, and meninges. The MCA supplies the remainder of the lateral cortex, including most of the frontal and parietal lobes, as well as the superior and medial portions of the temporal lobe, the basal ganglia, and the internal capsule (Caplan, 2022; Chong, 2022c; Franco, 2018).
Figure 2
Common Carotid Artery
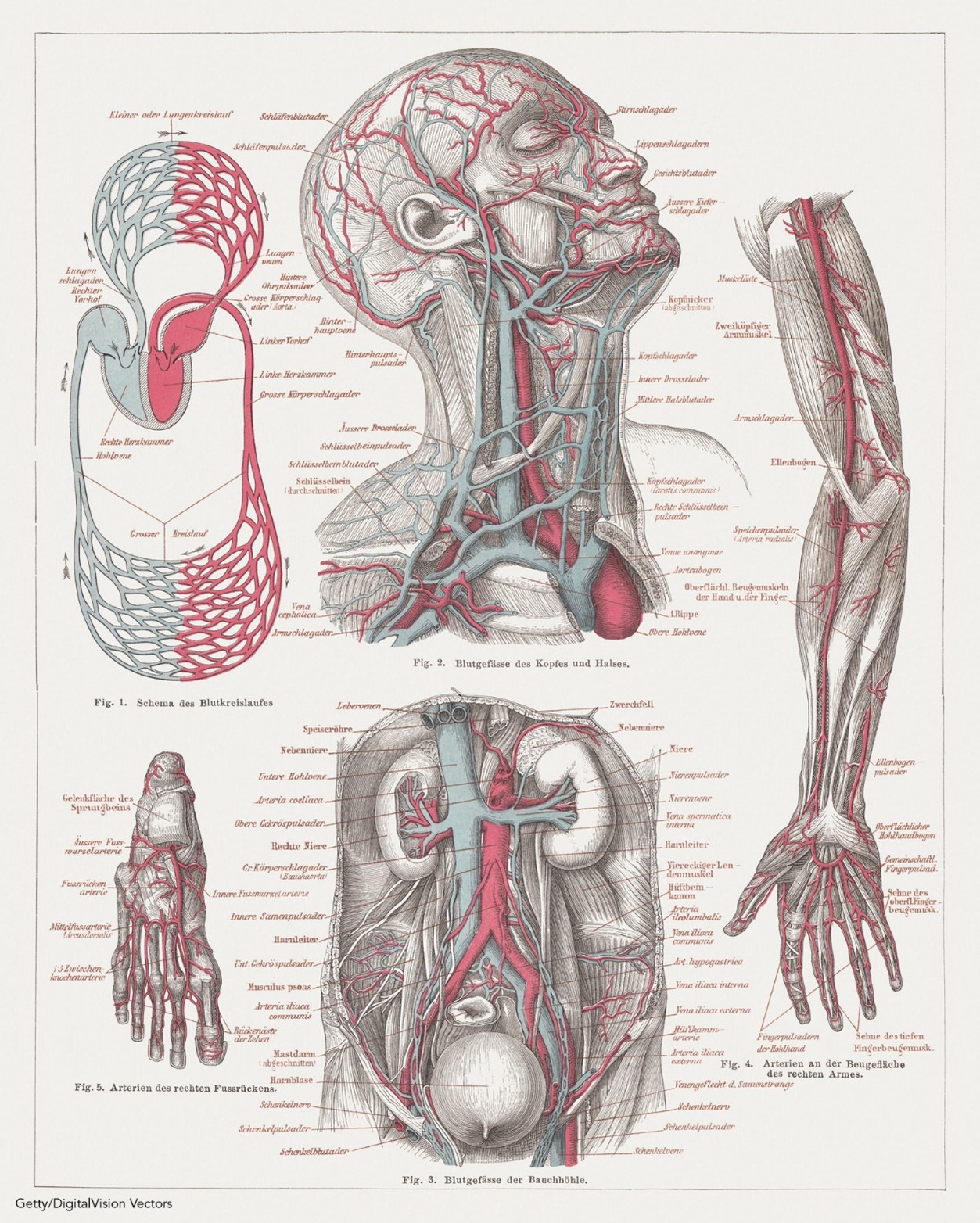
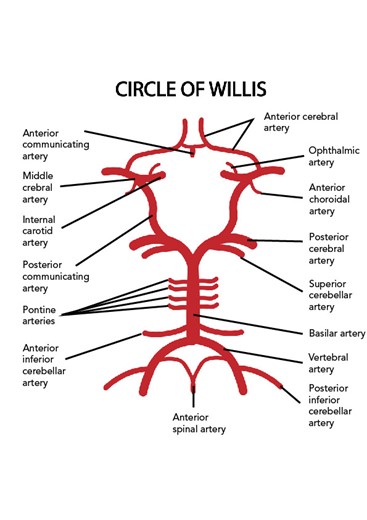
Posterior circulation starts with the vertebral arteries, which branch off of the subclavian arteries, and travel up through the transverse foramina of the cervical vertebra and the foramen magnum to supply blood to the cranial bones and meninges and converge to form the basilar artery. The basilar artery supplies blood to the pons, cerebellum, and inner ear. The basilar artery splits again into the posterior communicating artery to form the Circle of Willis (Figure 3), which surrounds the pituitary gland. However, only about 20% of the population has a complete arterial circle. The posterior cerebral artery then branches off to supply the inferior and medial portions of the temporal and occipital lobes, the midbrain, and the thalamus (Caplan, 2022; Chong, 2022c; Franco, 2018).
Figure 3
Circle of Willis
There are two main types of stroke: an ischemic stroke, where blood flow to an area is reduced to critical levels or stopped completely, and a hemorrhagic stroke, where abnormal bleeding occurs in an area of the brain. Ischemic strokes (Figure 4) can either be caused by a thrombus, which is a blood clot that forms in an artery that supplies blood to the brain, or an embolus, which is a blood clot, plaque, or fatty tissue that travels from somewhere else in the body (such as the heart or the peripheral vasculature) and becomes lodged in and blocks an artery that supplies blood to the brain. In both types of ischemic stroke, the plaque or clot keeps oxygen-rich blood from getting to a portion of the brain, and neurons deprived of oxygen start to die within minutes. Ischemic stroke is most commonly caused by atherosclerosis, a condition where plaque builds up along the walls of arteries. This plaque hardens and narrows arteries, and if it cracks or ruptures, it attracts platelets and eventually leads to blood clots. If a plaque formation breaks off into the artery, this can create an embolus downstream. Atrial fibrillation (Afib) is an irregular cardiac rhythm that allows for the pooling of blood in the atrium of the heart, which increases the risk of embolic stroke if a blood clot forms there and is then expelled and travels up to the brain (Caplan, 2022; Chong, 2022a, 2022b; Hui et al., 2022; National Heart, Lung, and Blood Institute [NHLBI], 2022b; Tadi & Lui, 2023).
Figure 4
Ischemic (Embolic) Stroke
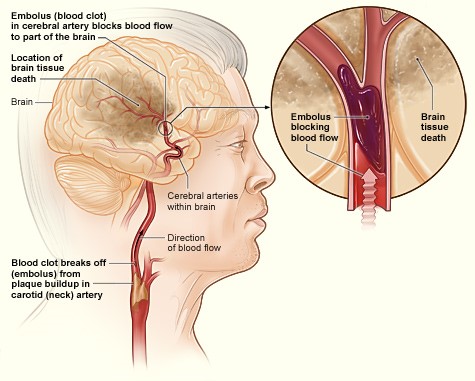
(NHLBI, 2013b)
A hemorrhagic stroke (Figure 5) can either be caused by bleeding into the parenchyma of the brain (intracerebral hemorrhage [ICH]) or in the space around the brain between the inner and middle membranes (subarachnoid hemorrhage [SAH]). In both types of hemorrhagic stroke, the blood causes swelling and cellular damage in the surrounding brain tissue and increased pressure within the skull, which is a closed container. SAHs are often caused by a ruptured aneurysm, a weakened bulge in an artery. ICHs may be caused by hypertension, trauma, or an arteriovenous malformation (AVM), an abnormal clustered connection of blood vessels between arteries and veins (NHLBI, 2022b). Medications (i.e., blood thinners, sympathomimetics), coagulopathy, and cerebral amyloid angiopathy may also cause...
...purchase below to continue the course
Figure 5
Hemorrhagic (ICH) Stroke
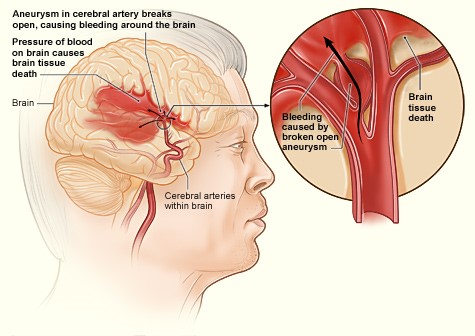
(NHLBI, 2013b)
Risk Factors and Prevention
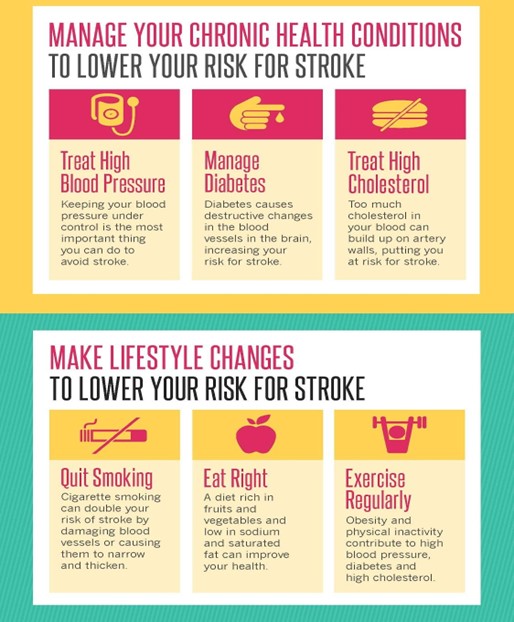
Stroke has both non-modifiable and modifiable risk factors. According to the American Heart Association (AHA)/American Stroke Association (ASA, 2014) guideline for the primary prevention of stroke, non-modifiable factors include age, gender, race, the presence of brain aneurysms or AVMs, low birth weight, and a family history of stroke. The risk of a stroke increases with age., doubling every 10 years after age 55. Although strokes are more common in adults over 65, one in seven strokes occurs in adolescents and young adults ages 15 to 49. In younger age groups, stroke is more common in men, but the mortality rate from stroke is higher in women. Younger women have a higher risk of stroke due to pregnancy and hormonal contraceptives. Stroke is also more common among certain racial groups, with non-Hispanic Black patients or Pacific Islanders having higher mortality rates from stroke than non-Hispanic White patients, Hispanic patients, American Indian patients, or Alaska Native patients. In addition, Black patients are twice as likely to have a first stroke and die from a stroke than White patients. Low birth weight is associated with an increased risk of stroke later in life. Research has found that babies born with low birth weight were twice as likely to have a stroke, myocardial infarction (MI), or develop heart disease by age 50 than babies born with normal birth weight. Genetics does play a role in the risk of having a stroke, with some genetic disorders (e.g., sickle cell anemia) increasing the risk of a stroke. Individuals with a family history of stroke also share common environmental exposures that could impact the risk of a stroke. In addition, individuals with a previous transient ischemic attack (TIA) have a higher risk of a stroke (CDC, 2023a; Meschia et al., 2014; Rost & Simpkins, 2023).
Modifiable risk factors for stroke include hypertension, dyslipidemia, diabetes, asymptomatic carotid artery stenosis, heart disease (such as coronary artery disease [CAD], cardiomyopathy, heart failure, and Afib), smoking, alcohol and drug use (i.e., more than one alcoholic drink per day, cocaine use, and IV drug use), vasculitis, lack of physical activity, being overweight/obese, chronically elevated stress, depression, unhealthy diet (i.e., high fat, high sodium, and low in fresh fruits/vegetables), and the use of certain medications, such as hormonal birth control and nonsteroidal anti-inflammatory drugs (NSAIDs). Smoking damages and tightens blood vessels, raising the risk of stroke. Of the modifiable risk factors listed above, the AHA reports that treating hypertension most significantly impacts risk reduction. A diagnosis of Afib may increase the risk of stroke by a factor of five. Other potentially modifiable risk factors include migraines, sleep-disordered breathing, hyperhomocysteinemia, infection, and inflammation (CDC, 2023a; Meschia et al., 2014; Rost & Simpkins, 2023; Tsao et al., 2023; Wandell et al., 2017).
There is also an increased risk of stroke for people who regularly experience extreme climates and those with lower incomes. As mentioned above, an increased risk of stroke-related death can also be seen in areas like the southeastern US "stroke belt." The theory is that the diet, lifestyle, and racial profiles common in this area of the country are responsible for this trend. Some less common medical conditions can increase the risk of stroke, such as fibromuscular dysplasia, septal defects such as patent foramen ovale (PFO), and erythrocytosis (increased red blood cell count). In children, congenital heart defects, immune disorders, arterial disorders, blood clotting disorders, head and neck trauma, maternal history of infertility, infection of the amniotic fluid, premature rupture of membranes, and maternal hypertension increase the risk for stroke (CDC, 2023a; Rost & Simpkins, 2023; Franco, 2018).
Primary Prevention
Given the many modifiable risk factors, prevention should be the first step in reducing the risk of a stroke. Primary prevention refers to treating and controlling modifiable risk factors to prevent a patient's first stroke. This prevention means actively and appropriately managing hypertension, diabetes, Afib, hypercholesterolemia, and other risk factors. Following a heart-healthy lifestyle, which includes regular exercise and a healthy diet (i.e., a diet high in fiber, fruits, vegetables, whole grains, and lean meat and low in saturated fats, trans fats, sodium, added sugar, and alcohol) can help to lower the risk of stroke. This approach may also include a weight loss program to maintain a healthy weight. Smoking cessation also decreases the risk of stroke and numerous other detrimental effects. Appropriately managing stress can also reduce the risk of stroke (CDC, 2022b; Franco, 2018; Hennekens, 2022).
The AHA (2017) published a guideline on the importance of self-care for stroke and other CVD prevention. Self-care is "whereby individuals and families maintain health through health-promoting practices and managing illness" (Riegel et al., 2017, p. 2). They break this down into three general categories: self-care maintenance, which includes maintaining physical and emotional stability; self-care monitoring, which includes observing oneself for changes in signs or symptoms (also called "body listening"); and self-care management, which includes appropriately responding to signs or symptoms if and when they occur. Other than the previously mentioned individual-level prevention techniques, stroke prevention programs should also assess and optimize positive family support as well as community-level prevention methods, including access to medical services, healthy food, open spaces, a safe environment, healthy air, regular physical activity, and social cohesion (Riegel et al., 2017).
Figure 6
Primary Stroke Prevention
(National Institute of Neurological Disorders and Stroke [NINDS], 2023)
Secondary Prevention
One in four stroke survivors will have another stroke within five years, and the risk of a stroke within 90 days of a TIA is as high as 17% (CDC, 2023b). Secondary prevention is preventing a recurrent stroke after an initial stroke or TIA. The ASA and AHA (2019) guidelines for the early management of acute ischemic stroke patients and the 2021 guidelines for the prevention of stroke in patients with a stroke or TIA both make recommendations for the secondary prevention of strokes. Secondary prevention strategies depend on the stroke or TIA subtype; therefore, the diagnostic workup to determine the etiology is essential to determining the treatment strategies for secondary prevention. Management of primary risk factors described above (i.e., diabetes, hypertension, hypercholesterolemia, and smoking) are essential and should be tailored to the individual patient. Lifestyle modifications (i.e., diet and exercise) often require behavioral change interventions. Cardiac monitoring is recommended to screen for Afib or other arrhythmias for at least the first 24 hours after a stroke, but the effectiveness of prolonged monitoring throughout hospitalization is uncertain. Prolonged monitoring may be suggested for unknown stroke etiology (Kleindorfer et al., 2021; Powers et al., 2019; Rost & Simpkins, 2023).
The 2021 AHA/ASA guidelines highlight the importance of timely evaluation of the stroke etiology to identify modifiable risk factors. Addressing hypertension, hypercholesterolemia, and diabetes is key to reducing the risk of a subsequent stroke or TIA. An echocardiogram is recommended to identify specific diseases, including PFO, endocarditis, intracardiac thrombi, and myxoma. Regarding patients who have had a stroke and have hypertension, after the initial 72 hours, it is safe and reasonable to initiate or restart antihypertensive medications before discharge if the patient's blood pressure is consistently above 140/90. Treatment with thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin II receptor blockers (ARBs) are recommended. Antiplatelet agents are recommended for patients with non-cardioembolic acute ischemic stroke (AIS) over oral anticoagulation. The combination of antiplatelets and anticoagulation is not recommended. In addition, dual antiplatelet therapy (DAPT) with aspirin (ASA) and clopidogrel (Plavix) is not recommended for short- or long-term treatment in those at higher risk of hemorrhagic conversion (high NIHSS score or large infarct). DAPT is recommended for minor stroke and high-risk TIA or severe symptomatic intracranial stenosis (Dong et al., 2020; Kleindorfer et al., 2021; Powers et al., 2019; Rost & Simpkins, 2023).
Patients with cardioembolic stroke related to a history of Afib should be started on oral anticoagulation medication within 4 to 14 days (if not already on) as a risk reduction measure to prevent another stroke. According to the ASA, the benefits of concurrent antiplatelet and anticoagulation therapy are uncertain in patients with comorbid CAD. Studies have shown that using anticoagulation medication(s), even combinations of two medications, in patients with Afib does not increase the risk of hemorrhagic stroke. However, the risk of death does increase in these patients if a hemorrhagic stroke does occur. In patients diagnosed with a stroke secondary to a vertebral or carotid artery dissection, secondary prevention with antiplatelet or anticoagulation medication for 3 to 6 months following the stroke is reasonable (Powers et al., 2019; Rost & Simpkins, 2023; Wandell et al., 2017). Those with TIA or AIS due to underlying Afib who cannot take an oral anticoagulant may be treated with DAPT (Dong et al., 2020).
For adults at least 20 years old not on lipid-lowering agents, measuring either a fasting or nonfasting plasma lipid profile can effectively determine ASCVD risk. Cholesterol levels should also be obtained after a stroke to assess the effectiveness of a previously prescribed statin medication. Continuation of statin medication in the acute phase following a stroke is reasonable, and high-intensity statin therapy is recommended in patients aged 75 and under following an acute stroke. Moderate-intensity therapy should be considered for patients over 75 following a discussion regarding the risks and benefits with the patient and family to make a well-educated and informed decision. Lifestyle and diet modification should be attempted in these patients as well. According to the AHA/ASA guidelines, it is reasonable to screen all patients for diabetes with fasting plasma glucose, hemoglobin A1C, or an oral glucose tolerance test following an ischemic stroke (Kleindorfer et al., 2021; Powers et al., 2019; Rost & Simpkins, 2023).
According to the AHA/ASA for the prevention of stroke in patients with a previous stroke or TIA (2021), noninvasive testing, such as computed tomography angiography (CTA), magnetic resonance angiography (MRA), or ultrasound, may guide the selection of appropriate secondary stroke prevention treatments for some patients with acute ischemic stroke (i.e., patients with carotid artery stenosis who are potential candidates for carotid revascularization whose neurologic examination does not permit accurate localization and patients with a PFO who are potential candidates for mechanical closure). If a patient is suspected or known to have had a non-disabling ischemic stroke in the carotid territory and may be a candidate for stent placement or carotid endarterectomy (CEA), noninvasive imaging of the cervical vessels should be performed within 24 hours of admission. However, the potential benefit of urgent or emergent CEA procedures in the acute phase following a stroke is not well established. Routine screening for obstructive sleep apnea (OSA), antiphospholipid antibodies, and hyperhomocysteinemia following a stroke is not recommended (Kleindorfer et al., 2021; Powers et al., 2019; Rost & Simpkins, 2023).
Many of the secondary prevention measures discussed here are also core/primary stroke clinical quality measures (CQMs) published by the Joint Commission (TJC), including the use of antiplatelet medication, anticoagulants, and lipid-lowering statin medications for secondary prevention following a stroke (TJC, 2023). A secondary prevention measure tested with some favorable results in stroke patients is repetitive bilateral arm ischemic preconditioning (BAIPC). This method aims to improve cerebral perfusion and thus decrease the risk of stroke recurrence and has been well-tolerated in patients (Zhao et al., 2018). In a study published by Meng and colleagues (2015), 58 patients over 80 were enrolled and randomized into an experimental or control group. The experimental group was instructed to perform five cycles twice daily of bilateral arm ischemia lasting five minutes per cycle for 180 days, starting about seven days following either a stroke or TIA, while the control group was given a sham exercise to perform. The experimental group (n=30) had two recurrent infarcts and seven TIAs during the study period, while the control group (n=28) had eight infarcts and 11 TIAs during the same period. The experimental group also showed decreased levels of c-reactive protein (CRP), interleukin-6, leukocytes, and a decreased platelet aggregation rate; they also developed increased tissue plasminogen activator (tPA) compared to the control group participants (Meng et al., 2015).
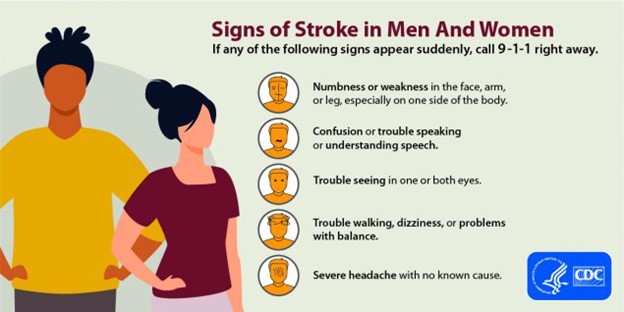
Stroke Signs and Symptoms
Signs and symptoms of a stroke can develop quickly (i.e., within minutes) or more slowly (i.e., over hours or days). The signs and symptoms will vary depending on the area of the brain that has been affected and will last for at least 24 hours. Symptoms of a stroke that resolve spontaneously in less than 24 hours, usually in one to two hours, are defined as TIAs (CDC, 2022a; Chong, 2022c; Hui et al., 2022). Common signs and symptoms of a stroke include:
- weakness, usually on one side of the body
- paralysis or numbness of the face, arms, or legs, usually on one side of the body
- confusion
- difficulty speaking or understanding speech
- vision changes in one or both eye(s)
- difficulty breathing
- dizziness
- difficulty walking or unexplained fall(s)
- loss of balance or coordination
- loss of consciousness
- sudden and severe headache (usually indicates a hemorrhagic stroke; CDC, 2022a; Chong, 2022c; Hui et al., 2022)
The importance of public education campaigns such as FAST (face, arms, speech, time to call 911) that target stroke education cannot be overstated (see Figure 7). The general public has a long-held inaccurate belief that strokes are not medical emergencies worthy of initiating the emergency management system (EMS). Patients should be informed that when signs or symptoms of a stroke are seen, the only acceptable response is to call 911 for ambulance transport to a hospital equipped to manage acute strokes. Aphasia is a common stroke symptom defined as difficulty understanding speech, speaking, reading, or writing language. It affects up to one-third of all stroke patients and is usually seen in strokes affecting the left side of the brain. Unfortunately, 30% to 40% of those diagnosed with aphasia symptoms immediately following a stroke develop chronic difficulties. Brainstem strokes that affect the pons are also called pontine strokes and account for 10% of all ischemic strokes. If severe enough, these can cause "locked-in syndrome," a complete lack of control of motor function except for the eyes but maintained cognitive function (CDC, 2022a; Franco, 2018; NHLBI, 2022a).
Figure 7
Campaign for Stroke Symptom Awareness
(CDC, 2022a)
Diagnosis and Management
Initial Management
Initial evaluation and treatment for stroke symptoms typically start with EMS providers. The AHA/ASA (2019) guidelines for the early management of patients with acute stroke state that EMS providers should have a stroke assessment system in place with treatment protocols and notification of the nearest stroke center hospital in hopes of delivering comprehensive specialized stroke care that incorporates rehabilitation. The primary objectives of prehospital care are airway management, cardiovascular support, and transport to the closest facility prepared to care for acute stroke patients (Powers et al., 2019).
Certification of stroke centers by independent, external organizations is recommended. TJC can give hospitals designations as an acute stroke-ready hospital (ASRH), a primary stroke center (PSC), a thrombectomy-capable stroke center (TSC), or a comprehensive stroke center (CSC). Each certification has designated requirements, and hospitals must apply and be reviewed for initial certification and continued certification or renewal (Powers et al., 2019; TJC, n.d.; Waldman et al., 2022).
- An ASRH must have an acute stroke team available 24 hours a day, initial evaluation by an emergency department (ED) physician, nurse practitioner (NP) or physician's assistant (PA), a neurologist available in person or via telemedicine 24 hours a day, neurosurgical services available within three hours, a transfer protocol established with at least one PSC or CSC, the ability to administer intravenous (IV) tPA and then transfer the patient safely to another facility, and document that they meet three inpatient and two outpatient stroke clinical performance measures (CPMs).
- A PSC must have all of the above, plus an initial evaluation by an ED physician, a designated unit or group of beds for acute care of stroke patients, the ability to manage a patient after receiving IV tPA, neurosurgical services within two hours with 24/7 operating room availability for neurosurgical services, and document that they meet eight core stroke CPMs.
- A TSC must have all of the above, as well as provide evidence that they have completed at least 15 thrombectomies over the last 12 months, a dedicated neurointensive care unit or beds available 24/7, magnetic resonance imaging (MRI), CTA, MRA, and catheter angiography available 24/7, ability to perform and manage mechanical thrombectomies and intra-arterial (IA) thrombolytics and document that they meet an additional five ischemic hemorrhagic comprehensive stroke CPMs.
- A CSC must demonstrate all of the above, as well as provide evidence that they have treated at least 20 SAH cases caused by aneurysm annually, including 15 endovascular coiling or microsurgical clipping procedures, managed IV thrombolytic therapy at least 25 times annually, neurologist and neurosurgical services accessible 24/7 in person with a written call schedule, ability to perform stenting of carotid arteries or CEA procedures, and document that they meet a total of eight core and ten comprehensive stroke CPMs.
Each category also has specific education requirements for the providers, nurses, and staff caring for acute stroke patients. Certification reviews range from one reviewer for one day in ASRHs to two reviewers for two days in CSCs (TJC, n.d.; Waldman et al., 2022).
Otherwise, the emergency care of a stroke patient also includes circulatory assessment (with chest compressions if necessary), airway assessment (and management if necessary), and breathing assessment (with ventilatory support if necessary), just as in any other medical emergency. A full history and physical exam, including a comprehensive neurological exam, should be completed quickly on any suspected stroke patient upon arrival to the ED. This assessment includes a history of risk factors, current signs or symptoms, and exactly when the symptoms began (if known). The physical and neurological exam should evaluate the patient's alertness, comprehension, coordination, balance, sensation, strength, speech, and vision. A quick check for an audible carotid bruit should also be included (Oliveira-Filho & Mullen, 2023; Tadi & Lui, 2023). In an ASRH, this initial full evaluation should be completed and documented by an ED physician, NP, or PA; in a PSC, TSC, or CSC hospital, it should be completed and documented by the ED physician. A neurologist is available 24/7 in a CSC hospital, but often the initial neurology consult may be completed via telemedicine in other lower-level hospitals, even PSC and TSC hospitals (TJC, n.d.).
For the acute management of patients with AIS, the guidelines recommend using supplemental oxygen only if the patient's oxygen saturation is less than 94%. Hypotension and hypovolemia should be corrected to help support optimal organ function by maintaining systemic perfusion. Blood pressure should be carefully lowered to below 185/110 before the fibrinolytic/invasive treatment of AIS. If no fibrinolytic therapy or endovascular procedures are possible, there is no benefit to initiating antihypertensives within the first 48 to 72 hours after the initial stroke as long as blood pressure is below 220/120. If above 220/120, it might be reasonable to lower the blood pressure by 15% in 24 hours. Sources of hyperthermia (temperature above 100.4 °F [38 °C]) should be identified and corrected; antipyretics should be given to lower the temperature to a normal range. Hyperglycemia should be treated to maintain a range of 140-180 mg/dL; hypoglycemia below 60 mg/dL should also be corrected. Poorly managed blood glucose levels can lead to poor outcomes in stroke patients. A serum blood glucose check is the only laboratory test recommended before administering IV tPA in an acute stroke patient (Powers et al., 2019).
Telemedicine is a cost-effective solution to provide stroke neurology expertise to every patient, regardless of where they may present to obtain care. It has been shown to significantly improve both short-term and long-term clinical outcomes and decrease disparities in the quality of care. A class I (strong) recommendation from the AHA/ASA guidelines (2019) is that hospitals develop a stroke protocol for patient evaluation and treatment by a trained and qualified Stroke Team. They also recommend using telemedicine/telestroke resources supported by healthcare institutions, governments, and payers to ensure adequate 24/7 coverage for acute stroke patients in various settings. The AHA/ASA guidelines also recommend that telestroke evaluation, a telehealth evaluation with a trained neurologist experienced in remote stroke diagnosis, can improve triage and accurate decision-making for IV tPA in stroke patients. Another recommendation based on nonrandomized data is that IV tPA administration within a telestroke network is as beneficial and safe as done within a stroke center hospital. Telestroke may also be reasonable for triaging patients with acute stroke who are potentially eligible for interfacility transfer for emergency mechanical thrombectomy (Powers et al., 2019).
Diagnosis
An initial evaluation of a potential ischemic stroke patient should also include a rating using a stroke severity scale, such as the National Institutes of Health Stroke Scale (NIHSS) (Powers et al., 2019). The NIHSS was first developed in 1983 to assess the neurological deficits present post-stroke, modified last in 1992, and takes approximately seven minutes to complete. It includes 11 items and produces a final score between 0 and 42. The higher the score, the worse the deficits. It assesses the patient's level of consciousness, gaze palsy, visual fields, facial palsy, bilateral upper extremity strength, bilateral lower extremity strength, limb ataxia, sensation, extinction/neglect/inattention, dysarthria, and language. A provider should be certified and trained to administer the NIHSS properly (Hui et al., 2022; Oliveira-Filho & Mullen, 2023).
Hemorrhagic stroke patients should also be evaluated with specialized tools. For SAH patients, the Hunt and Hess Scale is recommended for initial evaluation; the ICH score is recommended for patients with ICH. These should be completed before any surgical intervention to serve as a baseline measure, help inform prognosis, and facilitate effective communication between providers and facilities regarding patient severity and condition. The Hunt and Hess Scale provides a score that ranges from 1 (asymptomatic, mild headache, slight nuchal rigidity) to 5 (decerebrate posturing, coma). The ICH score considers the patient's Glasgow coma score (GCS), age, the volume of ICH, and whether there exists an infratentorial origin or an intraventricular hemorrhage on imaging. These are then combined into a numerical value ranging from 0 to 6, with a higher score indicating a worse prognosis or higher expected mortality rate (Greenberg et al., 2022; Rordorf & McDonald, 2023; Singer et al., 2021).
In addition to the NIHSS and other stroke scales used to initially evaluate a patient, two other stroke scales are commonly utilized later to assess residual or chronic deficits. The modified Rankin Scale (mRS) was originally introduced in 1957 by Dr. John Rankin. It is an interview-style evaluation that can be completed in person or over the phone. In most cases, it is traditionally performed 90 days after the stroke and takes approximately two minutes to complete. Scores range from 0 (no residual symptoms) to a maximum of 6 ( the patient is deceased as a direct result of the stroke). An mRS of 2 or less indicates functional independence. Another commonly used disability tool is the Barthel Index (BI), first published in 1965 and used similarly to the mRS. It is either an observational or interview-style tool that can be completed with a family member or caregiver. It assesses a patient's ability to complete ten different activities of daily living (ADLs) with a total score ranging from 0-100. The BI includes feeding, transferring from bed to chair and back, personal care/hygiene, getting on or off the toilet, bathing, walking, going up or down the stairs, dressing, bladder control, and bowel control. A higher score correlates with greater functional independence (Goldstein, 2023; Saver et al., 2021).
Imaging
If a stroke is suspected after a complete history and physical exam, the next step in evaluation is typically imaging studies. The imaging studies commonly ordered in stroke patients and their positive and negative features will be reviewed. Regarding imaging studies, the AHA/ASA guidelines (2019) recommend that all suspected stroke patients undergo diagnostic brain imaging before initiating any specific therapy to treat AIS, usually in the form of a non-contrast CT scan of the head. Ideally, at least 50% of stroke patients should receive this within 20 minutes of arrival at the ED. They strongly recommend a noninvasive intracranial vascular study during the initial imaging evaluation of a stroke patient if they are believed to be a candidate for endovascular treatment as long as this does not delay IV tPA administration. Systems should be established to ensure brain imaging is done as quickly as possible in patients who may be candidates for IV tPA or mechanical thrombectomy. A CT scan of the head without contrast is the most common imaging study ordered initially in suspected stroke patients. This study is quick, widely available, and allows radiologists and neurologists to rule out hemorrhage reliably. Disadvantages of a non-contrast CT are the high dose of radiation delivered during the exam, the lack of reliability in detecting an early infarct core (brain tissue identified on imaging as having both decreased blood flow and blood volume), and the variable ability to detect a stroke via CT scan depending on the expertise level of the radiologist, the size and acuity of the stroke, and the window and level settings (Franco, 2018; Powers et al., 2019).
A non-contrast head CT is also used to determine a patient's Alberta Stroke Program Early CT Score (ASPECTS), which is used as a criterion for certain treatment options and can help predict stroke severity and functional independence. Scores range from 0-10; a lower score indicates a more pervasive and severe stroke. The main application of the ASPECTS is to identify patients with AIS who have a limited extent of early infarction (score ≥ 6) and who may be eligible for mechanical thrombectomy. Recently, mobile CT scanners have been constructed to reduce the time to treatment by up to 42 minutes. These look like large ambulances equipped with a CT scanner inside that function by scanning potential patients for a stroke while en route to the hospital. CTA creates a three-dimensional (3D) computer-generated reconstruction of a patient's entire intra- and extracranial circulation from the aorta to the Circle of Willis secondary to a timed, rapid injection of iodinated IV contrast in less than 60 seconds. The exposure to contrast is not without risk; however, patients with a known allergy to iodine or iodinated contrast or renal insufficiency (glomerular filtration rate [GFR] less than 30) should not receive iodinated contrast. Despite this, the AHA/ASA guidelines state that serum creatinine is unnecessary to assess before performing a CTA on an acute stroke patient with no history of renal impairment. A CTA can show any major artery occlusions and "spot signs," which indicate active bleeding and can predict hematoma expansion. A moderate recommendation from the AHA/ASA is to simultaneously include the carotid and vertebral arteries in the initial imaging study. However, as previously mentioned, the evidence supporting emergent or urgent carotid endarterectomy procedures post-stroke is not well established (Franco, 2018; Oliveira-Filho & Lansber, 2023; Powers et al., 2018).
CT perfusion studies use the same process as the CTA above but with the addition of specialized computer software that then determines the mean transit time to establish a penumbra (an area of brain tissue at risk for hypoxic damage but still currently salvageable if treated quickly, as it has decreased blood flow but normal blood volume on imaging). The disadvantages of a CT perfusion study include the radiation exposure and contrast administration mentioned above and the expensive software needed to process the images. According to the AHA/ASA (2019), perfusion imaging should not delay IV tPA administration. They found no benefit to performing CT perfusion images in acute stroke patients within the six-hour time window from symptom onset for patient selection for mechanical thrombectomy procedure. These imaging studies are strongly recommended in acute stroke patients with large vessel occlusions in the anterior circulation that are between 6 to 24 hours from symptom onset, as these studies may be crucial in treatment decision-making in this group (Franco, 2018; Powers et al., 2019).
MRIs of the brain are also commonly used to evaluate stroke patients. Some consider them to be radiographically superior to CT scans in the acute phase. Additionally, they do not expose the patient to radiation and are recommended by the American College of Radiology. However, they take longer than CT scans to complete and thus have the risk of delaying treatment. MRI machines are also generally less available than CT scanners. The small area inside the machine commonly causes patients discomfort and anxiety related to claustrophobia, and there are several contraindications to MRI scans (i.e., the presence of certain aneurysm clips, pacemakers, defibrillators, stimulators, and shrapnel or other metal fragments in the eyes). They are recommended in cases of uncertain diagnosis and considered more sensitive for TIA cases. The American Academy of Neurology officially recommends an MR diffusion-weighted study in the first 12 hours after stroke symptoms develop as they find them more useful than CT scans (Franco, 2018; Oliveira-Filho & Lansberg, 2023; Powers et al., 2019). However, the consensus is that if obtaining an MRI scan will significantly delay treatment, then a CT scan is preferred (Franco, 2018; Oliveira-Filho & Lansberg, 2023; Powers et al., 2019).
- MRI diffusion-weighted images (DWI) take approximately ten additional minutes to complete and have been shown to detect early ischemic changes with better accuracy (99% sensitivity and 92% specificity).
- An MR perfusion study, similar to a CT perfusion study, utilizes a contrast agent (gadolinium) and a rapid series of MR images to detect a diffusion/perfusion mismatch (penumbra); this piece of information is especially crucial in patients that have had symptoms beyond the ideal treatment window. This imaging offers providers additional information regarding the potential utility of IV tPA therapy and/or interventional thrombectomy procedures. Patients with a gadolinium allergy, pregnant patients, or those with renal insufficiency should not receive gadolinium contrast. As previously mentioned, the AHA/ASA found no benefit to performing MR perfusion or DW-MRI within six hours of acute stroke symptom onset. Instead, these are useful for selecting candidates for mechanical thrombectomy between 6 to 24 hours of symptom onset.
- If unable to perform MR perfusion with IV contrast, arterial spin labeling can visualize brain perfusion by magnetically labeling (inverting) arterial blood protons.
- MR angiography can be used to image the vessels in the neck using IV contrast. It helps detect atherosclerotic lesions in the neck and head with increased reliability (sensitivity 85%) compared to a standard MRI but less than a CTA. It can visualize carotid or vertebral artery dissections or fibromuscular dysplasia.
- A "time-of-flight" MRA can image the major arteries of the head without using IV contrast.
If it is unknown whether a patient has MRI-compatible aneurysm clips, a pacemaker, metal eye fragments, or other contraindications to receiving an MRI scan, an x-ray of the head, chest, and abdomen can be done to help determine eligibility (Franco, 2018).
Management of Patients with Hemorrhagic Stroke
The AHA/ASA updated the published guidelines for managing patients with ICH in 2022. The guidelines highlight the importance of healthcare system organization and preparation to provide initial ICH care and, when appropriate, provide rapid transfer to facilities with neurocritical care. A baseline severity score (using the ICH score if the patient has an altered level of consciousness or NIHSS if the patient is conscious) and rapid neuroimaging to diagnose the problem are just as important for patients with hemorrhagic strokes as they are for patients with ischemic strokes. Vital signs, a complete history, and a targeted physical exam will help direct immediate care. Treatment for patients with ICH includes supportive measures, control of modifiable risk factors, and possible surgical evacuation. Routine laboratory work should include a complete blood count (CBC), creatinine/estimated GFR, glucose, cardiac troponin, electrocardiogram (ECG), toxicology screen, and inflammatory markers. In addition, coagulation factors and a platelet count should be ordered to assess for a coagulation factor deficiency, thrombocytopenia, or other abnormalities so these things can be addressed (Chong, 2022a; Greenberg et al., 2022; Unnithan et al., 2023).
A patient with severe hypertension (i.e., systolic blood pressure [SBP] 150-220 mmHg) with a mild-moderate hemorrhagic stroke needs antihypertensive medication to safely reduce their SBP to 140 to help limit the bleeding (with a maintenance goal of 130 to 150 mmHg), with vigilant control of blood pressure going forward. Careful titration is critical to ensure continuous smooth, and sustained control, avoiding peaks and large variability in SBP. Antihypertensive treatment should begin within 2 hours of ICH onset and reach the target SBP within 1 hour to reduce the risk of hemorrhage expansion and mortality. Lowering the SBP below 130 can be harmful. The safety and efficacy of lowering the SBP are not well established for patients with a large ICH or those requiring surgical decompression. The current guidelines do not specify an ideal antihypertensive but instead suggest a rapid onset and short duration for ease of titration and control of BP. They mention that intravenous nicardipine (Cardene), a calcium channel blocker, is a reasonable choice but that venous vasodilators (e.g., nitrates) should be avoided due to the unopposed venodilation (Chong, 2022a; Greenberg et al., 2022; Unnithan et al., 2023).
The AHA/ASA guidelines recommend that any patient with anticoagulant-associated ICH should have immediate discontinuation and rapid reversal of anticoagulation to improve survival. Coagulation factor deficiencies should be treated with factor replacement therapy and thrombocytopenia with platelets. In patients with vitamin K antagonist (VKA)-associated (i.e., warfarin [Coumadin]), spontaneous ICH and an INR ≥ 2.0, 4-factor (4-F) prothrombin complex concentrate (PCC) is recommended in preference to fresh frozen plasma (FFP) to achieve rapid correct of INR and reduce the risk of hemorrhage expansion. IV vitamin K should also be administered directly after coagulation factor replacement (PCC) to prevent a later increase in INR and hemorrhage expansion. For patients whose INR is 1.3 to 1.9, PCC administration may be reasonable to achieve rapid INR correction and prevent hemorrhage expansion (Greenberg et al., 2022).
In patients taking direct oral anticoagulation (DOAC)/direct Xa inhibitor medications such as dabigatran (Pradaxa), apixaban (Eliquis), or rivaroxaban (Xarelto), the AHA/ASA guidelines recommend evaluation of the activated partial thromboplastin time (aPTT) and prothrombin time (PT) and consultation with a hematologist. If the DOAC was taken within the previous few hours, activated charcoal might be reasonable to prevent absorption. For patients with direct Xa inhibitor-associated ICH, andexanet alfa (Andexxa) will reverse anticoagulation, and 4-F PCC or activated PCC (aPCC) may be considered to improve homeostasis. For patients with dabigatran (Pradaxa)-associated ICH, idarucizumab (Praxbind) is reasonable to administer for anticoagulation reversal. If idarucizumab (Praxbind) is unavailable, aPCC, PCC, or renal replacement therapy (RRT) may be considered. Finally, for patients with unfractionated heparin (UFH)-associated ICH or low molecular weight heparin (LMWH)-associated ICH, IV protamine sulfate is reasonable to reverse or partially reverse the anticoagulation effects (Greenberg et al., 2022).
Standardized protocols should be used for any patients with ICH. In addition, a formal dysphagia screening protocol should be ordered before oral intake to reduce the risk of aspiration pneumonia. Continuous cardiac monitoring for the first 24 to 72 hours after an ICH is reasonable to evaluate for cardiac arrhythmias. The AHA/ASA guidelines recommend that nonambulatory patients with ICH use sequential compression devices (SCDs) to prevent deep vein thrombosis (DVTs) starting on the day of hospital admission, but compression stockings alone are ineffective. In addition, nonambulatory patients may need low-dose UFH or LMWH to reduce the risk of a pulmonary embolism (PE) starting 24 to 48 hours after the ICH onset. Compression stocking alone is not sufficient for venous thromboembolism (VTE) prophylaxis. Glucose monitoring should be initiated, and treating hypoglycemia (< 40 to 60 mg/d) and hyperglycemia (> 180 to 200 mg/d) is recommended to reduce mortality (Greenberg et al., 2022).
Antiepileptic drugs (AEDs) are recommended in patients with clinical seizures or those with a change in mental status who are found to have electrographic seizures on electroencephalography (EEG) but should not be given prophylactically. Patients with ICH should be cared for in an intensive care unit (ICU) or a dedicated stroke unit with physicians and nurses trained in their specialized care. If deteriorating neurologically, patients with cerebellar hemorrhage and subsequent brainstem compression and/or hydrocephalus related to ventricular obstruction should have spinal fluid diversion with a ventriculostomy or lumbar drain and/or surgical removal of the hemorrhage as soon as possible. If an AVM is found to be the cause of the patient's stroke, the AVM can be removed surgically, or a liquid tissue adhesive can be injected into the AVM to block blood flow and stop the bleeding. Radiation can also be used to treat AVMs if they are found non-emergently and are not actively bleeding (Chong, 2022a; Franco, 2018; Greenberg et al., 2022; National Institute of Neurological Disorders and Stroke [NINDS], 2023b; Unnithan et al., 2023).
Figure 8
Brain Aneurysm
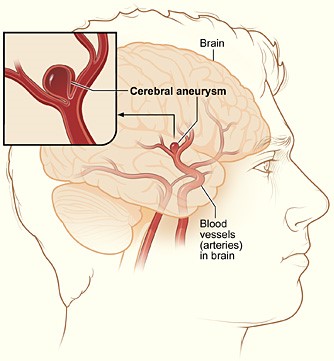
(National Institute of Health [NIH], 2010)
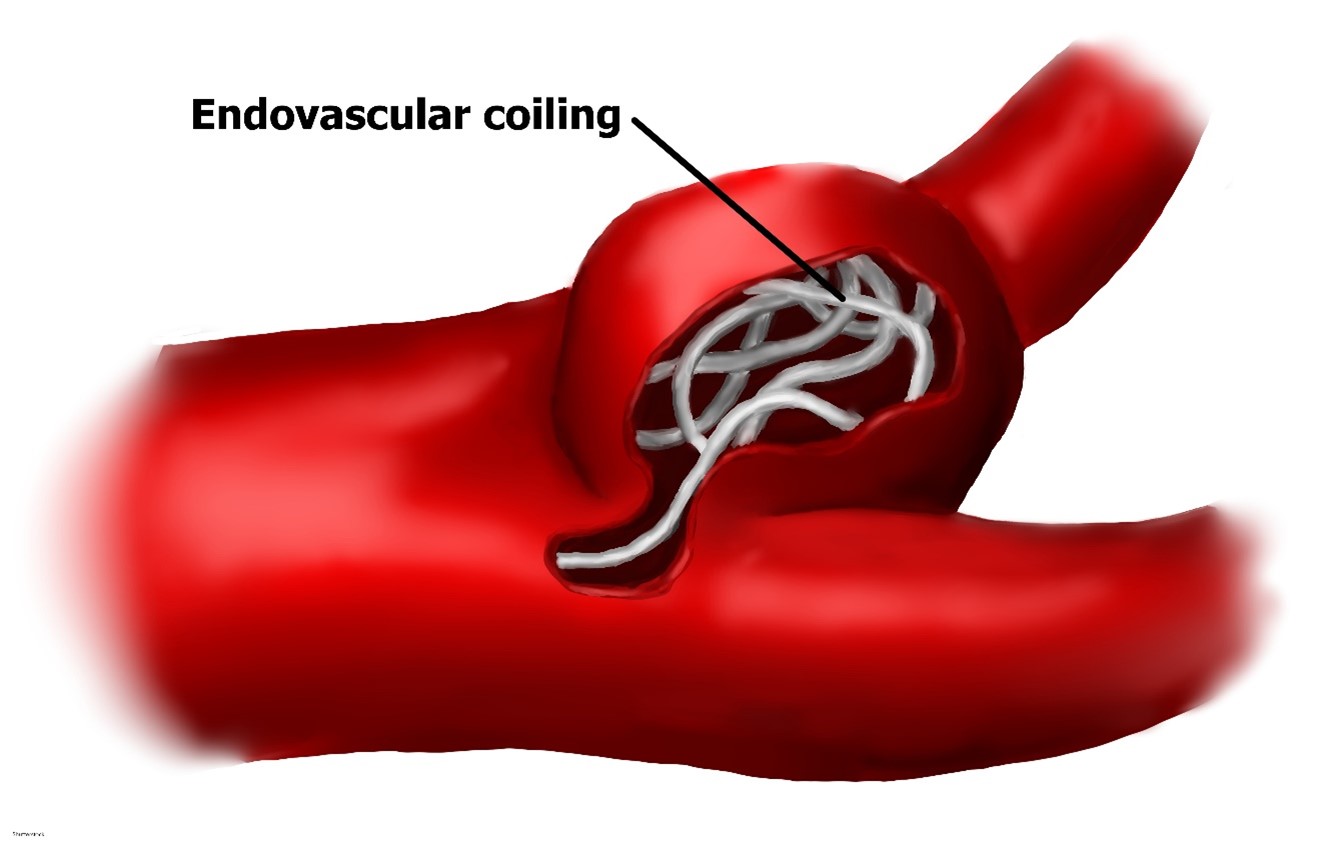
SAHs are most commonly associated with an aneurysm (Figure 8) that has ruptured or is leaking. An aneurysm may be treated surgically using microvascular clips placed at the base or neck to prevent future leaking by blocking it from blood flow. The risks are high for this procedure, as it requires open brain surgery to place the clips, but there is less risk of recurrence and repeat procedures in the future if done properly. Coil embolization (Figure 9) uses an access catheter placed in the groin to embolize an aneurysm with detachable platinum coils. It is less invasive than clipping but may need to be repeated in the future and is more likely to lead to the complication of cerebral vasospasms postoperatively. Three large randomized, prospective studies have compared both techniques. Of these, the International Subarachnoid Aneurysm Trial (ISAT) found a statistically significant improvement in survival rates at 12 months with coiling. This has strongly influenced surgical patterns in the last 15 years since its initial publication in the early 2000s. The most recent guidelines published by the AHA/ASA regarding aneurysmal SAH also recommend coiling over clipping when both are feasible. These procedures can also be done preventatively, depending on the location of the aneurysm. Larger aneurysms in the posterior circulation are more prone to rupture, and surgeons are more likely to recommend prophylactic surgical treatment if these are found non-emergently. The severity of the hemorrhage and the patient's age remain the two most important prognostic factors in aneurysmal SAH patients. A third surgical option for larger and more difficult-to-treat aneurysms is placing a stent-like flow diversion device via an endovascular catheter (Franco, 2018; Greenberg et al., 2022; NINDS, 2023b; Singer et al., 2023).
Figure 9
Cerebral Aneurysm Coiling Technique
Fibrinolytic Therapy and Thrombectomy Devices for Ischemic Strokes
IV tPA was first approved for therapeutic use in 1995 by the US Food and Drug Administration (FDA) and remains only approved for IV use. The patient's blood glucose should be checked before initiating IV tPA and corrected if necessary. Baseline troponin and an electrocardiogram (ECG) are recommended but not required and should not delay administration. Blood pressure should be carefully lowered to below 185/110 before initiating IV fibrinolytic therapy or a thrombectomy procedure (Powers et al., 2019; Tadi & Lui, 2023).
Treatment is time-dependent and thus should be initiated as soon as possible. In patients with acute stroke within three hours of symptom onset, IV fibrinolytic therapy with tPA (Alteplase; [Activase]) is recommended in patients over 17 with severe or mild but disabling stroke symptoms. Based on level B evidence, there is also a strong recommendation that patients with an acute stroke within three to four-and-a-half hours of initial symptom onset that otherwise meet the criteria should also be treated with IV tPA (Alteplase; [Activase] Powers et al., 2019; Tadi & Lui, 2023). The additional criteria suggested for patients within the three- to four-and-a-half-hour window include the criteria mentioned above, as well as:
- age 80 or less
- no history of prior stroke
- no history of diabetes mellitus
- NIHSS of no more than 25
- not taking an oral anticoagulant
- without imaging evidence of ischemic injury involving more than one-third of the MCA territory (Powers et al., 2019; Tadi & Lui, 2023)
IV tPA (Alteplase; [Activase]) should not be given with abciximab (Reopro, an antiplatelet medication) or within 24 hours of LMWH, such as enoxaparin (Lovenox). There is no need to check coagulation studies or platelet count before administration unless there is suspicion that these are abnormal. The risks and benefits of IV thrombolytic therapy should be extensively reviewed with the patient and family or caregivers, and staff and providers should be prepared and fully capable of managing any emergent adverse effects such as bleeding or angioedema (Powers et al., 2019; Tadi & Lui, 2023). Treatment should be stopped, and a head CT obtained immediately if the following symptom changes occur during or after IV tPA administration:
- severe headache
- acute hypertension
- nausea/vomiting
- a worsening or changed neurological exam (Powers et al., 2019; Tadi & Lui, 2023)
IV tenecteplase (TNKase) may be an alternative in patients with no major intracranial occlusion and only minor neurological impairment. It is recommended to avoid other concurrent treatments that could cause bleeding issues during administration, such as nasogastric (NG) tubes, urinary catheters, and intra-arterial pressure catheters, if they can be safely avoided. IV tPA is contraindicated in patients with acute intracranial hemorrhage on CT scan, a history of severe head trauma in the last three months, symptoms consistent with infective endocarditis or aortic arch dissection, or coagulopathy (platelets < 100 000/mm3, INR > 1.7, aPTT > 40s, or PT > 15s). IV tPA may be potentially harmful in patients with a history of AIS in the last three months, any history of ICH, signs/symptoms of SAH, a structural gastrointestinal (GI) malignancy, a recent bleeding event within 21 days, use of a thrombin inhibitor/factor Xa inhibitor within the previous 48 hours, an intra-axial intracranial neoplasm, or intracranial/intraspinal surgery in the last three months (Powers et al., 2019; Tadi & Lui, 2023).
A disadvantage of IV thrombolytic therapy is its lack of effectiveness in clearing large vessel occlusions. This, in combination with its very narrow window of availability, led researchers to continue developing stroke treatments that would improve upon these shortcomings. Intra-arterial injections of urokinase and prourokinase were developed and tested for safety and effectiveness in the PROACT I and II trials. PROACT II was published in 1999 and was a randomized trial testing recombinant prourokinase versus placebo in angiographic-documented proximal MCA occlusions. The trial showed increased recanalization and improved outcomes with acceptable complication rates, but the medication did not receive FDA approval. It does continue to be used, along with intra-arterial tPA and abciximab (Reopro), in an off-label capacity (Spiotta et al., 2015).
Following intra-arterial injections, researchers focused on interventional endovascular thrombectomy devices and other approaches to disrupt or remove the clot. The first attempt was a "J" or "C" shaped microwire for clot disruption. In 2005, the flexible intracranial balloon catheter was introduced. Although initially designed for vessel angioplasty, it was eventually used for mechanical thrombectomy by repeated angioplasty of the clot. Intracranial stents were developed next, including a partially deployed stent, such as the Enterprise vascular reconstruction device, that could either be placed permanently or partially deployed and retrieved, creating clot disruption and partial flow restoration. The downside of permanent stent deployment is the lifelong need for DAPT (Spiotta et al., 2015).
In 2004, the Mechanical Embolus Removal in Central Ischemia (Merci) retriever device became the first device cleared by the FDA for mechanical thrombectomy in acute stroke patients. It utilizes a corkscrew wire/suture tip to remove the clot en bloc. Revascularization rates range from 48% to 68%, and up to 36% of patients in initial studies reported a modified Rankin score (mRS) of 2 or less at 90 days. The Outreach distal access catheter (DAC) was approved in 2010; it provides buttressing access for Merci and similar devices to improve stability and aspiration power (Spiotta et al., 2015).
Then, in 2008 the Penumbra aspiration system was introduced. The Penumbra macerates the clot with a separator, which is repeatedly advanced into and withdrawn from the clot, all under direct suction. It utilizes a relatively large-bore catheter versus Merci's microcatheter. Studies of the Penumbra indicate revascularization rates between 82% to 87%, with up to 41% of patients reporting an mRS of 2 or less at 90 days. The Penumbra studies also report slightly lower complication rates than the Merci. Over time, the catheters used with the Penumbra device have improved, decreasing average procedure time. An advantage of the Penumbra device is that once the catheter has reached the target vessel, separator clot maceration can be performed without having to re-access (additional passes), as with the Merci device. In 2012, Penumbra introduced their Max series, which allows direct aspiration without a separator, decreasing the cost, and larger inner diameters at the distal and proximal end of the catheter, increasing the aspiration power. The Penumbra 3D separator attempts to engage the clot at the center of the vessel lumen with four intraluminal chambers (Spiotta et al., 2015).
Finally, the most recent development in thrombectomy devices is the stent retriever device, such as the Solitaire and Trevo Pro. These are now the most commonly used, and they are based on the earlier partially deployed stents, such as the Enterprise. These stents are removable, negating the need for long-term DAPT. The stents are opened from within the center of the thrombus, and suction is applied during retrieval; alternatively, they can be used with the Penumbra system for retrieval. Studies have shown the recanalization rates are superior to the Merci device (61% and 86% for Solitaire and Trevo, respectively), as are the mRSs (mRS of 2 or less at 90 days, 36% and 40% for Solitaire and Trevo, respectively; Spiotta et al., 2015). The AHA/ASA does not recommend devices to augment cerebral blood flow, neuroprotective agents such as magnesium, or transcranial near-infrared laser therapy (Powers et al., 2019).
One of the largest advantages of a mechanical thrombectomy procedure is that it is safe in patients with acute stroke within six hours of symptom onset. AHA/ASA guidelines (2019) stipulate that to qualify for mechanical thrombectomy with a stent retriever, a patient with AIS should meet all of the following criteria:
- mRS pre-stroke of 1 or less (no significant disability present)
- occlusion of the internal carotid artery or segment 1 of the MCA
- NIHSS score of 6 or greater
- at least 18 years of age
- ASPECTS of 6 or greater (Powers et al., 2019; Tadi & Lui, 2023)
The AHA/ASA guidelines have concluded that it is reasonable to proceed with thrombectomy in "carefully selected patients" with an occlusion in segment 2 or 3 of the MCA, the anterior cerebral artery, vertebral artery, basilar artery, the posterior cerebral artery, or those patients with a pre-stroke mRS of more than 1, an ASPECTS under 6, or an NIHSS under 6. If the patient presents with symptoms for 6 to 16 hours, they also recommend a thrombectomy procedure if the patient can meet DAWN or DEFUSE3 criteria or 16 to 24 hours if the patient meets the DAWN criteria (Powers et al., 2019). The DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention with Trevo (The DAWN Trial) published in 2018 shows that among the 207 patients enrolled in the study, the group who underwent thrombectomy had significantly improved functional outcomes based on mRS scores, with no significant difference in mortality or hemorrhage complication rates. The enrolled patients had stroke symptoms lasting between 6 and 24 hours secondary to acute occlusion of the intracranial ICA or proximal MCA. All patients had to have an NIHSS of at least 10. If 80 or older, they also had to have an infarct volume, as measured by DW-MRI or perfusion CT scan, of less than 21 mL. If under the age of 80, they had to have an infarct volume of less than 31 mL, or if their infarct volume was between 31 and 50 mL, they could qualify with an NIHSS of 20 or higher (Nogueira et al., 2018).
The Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke (The DEFUSE3 Trial) enrolled 182 patients with proximal MCA or ICA occlusions. The time limit for symptom duration for this study was between 6 to 16 hours. Patients were required to have an initial infarct volume (ischemic core) of less than 70 mL, a ratio of the volume of ischemic tissue to initial infarct volume of 1.8 or more, and an absolute volume of potentially reversible ischemia (penumbra) of 15 mL or more. Both studies utilized the same RAPID software to help calculate volumes based on DW-MRI or perfusion CT scans (Albers et al., 2018).
Post Procedure Care
After administration of IV tPA, the patient should be monitored closely for changes in neurological status, with blood pressure checks and a neurological exam every 15 minutes for the first two hours, then every 30 minutes for six hours, then hourly until 24 hours after initial administration of the medication. Neuroimaging should be repeated approximately 24 hours following the administration of thrombolytics before starting an oral antithrombotic agent. A blood pressure of less than 180/105 should be maintained for at least 24 hours following either administration of IV fibrinolytic or an endovascular thrombectomy. Blood pressure over this during the first 24 hours should be treated to avoid hemorrhagic conversion. In patients not treated with endovascular procedures or IV tPA, blood pressure can increase to as high as 220/120 for the first 48 to 72 hours after an acute ischemic stroke. For blood pressure over 220/120, it is reasonable to decrease it pharmacologically by 15% within 24 hours. Vasodilatory agents (i.e., nitrates) are not recommended. If the blood pressure consistently remains over 140/90, initiating or restarting an oral antihypertensive before discharge is safe and reasonable. Cardiac monitoring is recommended for at least 24 hours to rule out atrial fibrillation or another arrhythmia. In stroke patients with a diagnosis of Afib, anticoagulation therapy should be started within 4 to 14 days (Powers et al., 2019).
Regular skin assessments and optimal skincare (consistent turning, good hygiene, specialized mattresses/wheelchair cushions) are important to maintain skin integrity in patients with limited mobility. A dysphagia (difficulty swallowing) screen should be performed before allowing any oral intake in a stroke patient, preferably by a speech and language therapist (SLT). An enteral diet should be started within seven days of admission. If the patient has significant dysphagia, then a nasogastric (NG) tube (for short-term dysphagia) or a percutaneous endoscopic gastrostomy (PEG) tube (for longer-term dysphagia) should be placed to achieve this. Nutritional supplementation and oral hygiene are reasonable. Daily acetylsalicylic acid (ASA, Aspirin), adequate hydration, and SCDs are recommended for patients with immobility to reduce the risk of DVT. For non-cardioembolic strokes, urgent anticoagulation is not recommended. However, DAPT is recommended for the first 21 days (usually started within 24 to 48 hours if there is no tPA, 48 to 72 hours if the patient received tPA), followed by clopidogrel (Plavix) until 90 days in those with minor stroke or high-risk TIA to reduce the risk of recurrent stroke. Those with severe intracranial stenosis should receive DAPT for 90 days, and those with risk factors for hemorrhagic conversion (high initial NIHSS score or large infarct) should not receive DAPT. The AHA/ASA found no benefit to prophylactic antibiotics, and routine urinary catheter placement should be avoided. If they occur in acute stroke patients, seizures should be treated as they would otherwise, with AEDs chosen based on the patient's situation. AEDs should not be given prophylactically (Dong et al., 2020; Powers et al., 2019).
Symptomatic ICH occurs in 2% to 7% of patients with AIS after IV tPA treatment. This diagnosis is based on radiological findings and neurological exam changes. They typically occur within 36 hours of tPA administration. The neurological exams following an AIS treated with IV tPA are key, with thorough and complete documentation of any changes in the patient's NIHSS. Once identified, the patient should be moved immediately to an ICU or back to the stroke unit if not already there. Management includes cardiovascular/respiratory support if needed, blood pressure management, close neurological monitoring, prevention of hematoma expansion, and treatment of elevated intracranial pressure (ICP) and other complications that arise from the hemorrhage, including seizures, as with any spontaneous ICH (see the previous section on management of ICH). Based on the current research, a fibrinogen level should be sent while empirically transfusing 10 units of cryoprecipitate; cryoprecipitate should be transfused as needed to achieve a fibrinogen level of at least 150 mg/dL. Platelets may also be transfused, especially if the patient's platelet level is under 100,000/μL. FFP, PCCs, and/or vitamin K may also be considered in patients previously on warfarin (Coumadin). Two antifibrinolytic agents, aminocaproic acid (Amicar) and tranexamic acid (Cyklokapron), may also be considered, but the AHA/ASA suggests further research to identify when they are best utilized. They may be helpful in patients who refuse blood products as they work by inhibiting proteolytic enzymes such as plasmin, which are known to mediate the action of alteplase. Due to complications, rFVIIa should be avoided in spontaneous ICH (Yaghi et al., 2017).
Other common complications following an acute stroke include cerebellar or cerebral edema, which may lead to obstructive hydrocephalus, especially in cerebellar infarcts. Patients with large supratentorial infarcts are also at increased risk for cerebral edema leading to increased ICP. This risk should be communicated with the patient and family, and treatment and care options should be discussed early. Measures should be taken to reduce the risk of edema, and patients should be monitored closely for signs or symptoms. Osmotic therapy and brief moderate hyperventilation (PCO2 target 30 to 34 mmHg) are medical treatments that are reasonable for cerebral or cerebellar edema, but hypothermia, barbiturates, and corticosteroids should be avoided. Patients with large infarcts should be transferred to a care facility with neurosurgical expertise if needed. According to the AHA/ASA guidelines, ventriculostomy is the treatment of choice; a decompressive craniectomy may become necessary. A lumbar drain could also be considered if short-term spinal fluid diversion is needed postoperatively (as is common in SAH patients). Decompressive craniectomy reduces mortality in stroke patients under 60 with a unilateral MCA infarct with continued neurological deterioration for 48 hours after acute stroke. A craniectomy may be considered for patients over 60, as it has still been shown to reduce mortality by as much as 50% in this older group but has less favorable outcomes on functional recovery. The AHA/ASA specifically recommends stroke education, provided to both the family and the patient, allowing the patient to talk about the impact of the illness on their lives (Powers et al., 2019).
Finally, a note regarding teamwork, protocols, and workflow optimization is important to include here as a final umbrella that affects all stages of care for patients with a stroke. The AHA/ASA recommends throughout the guidelines that hospitals and providers develop organized protocols and designate teams to provide comprehensive specialized care to patients with a stroke. While these recommendations may not be as interesting to focus on as new technology, devices, and pharmaceuticals, they are exceedingly important (Powers et al., 2019). A German hospital conducted a study published in 2018 regarding the effect of two significant changes on how they care for patients with an acute stroke. The first change was to provide 24-hour, on-site neuroradiological service. This change provided some improvement in their outcomes but was not statistically significant. Only after they instituted extensive workflow optimization and documentation of procedure times did they see significant improvements in their door-to-image, image-to-puncture, and door-to-revascularization times, especially in patients presenting for care outside normal business hours (Nikoubashman et al., 2018).
Rehabilitation
After a stroke, there are two primary mechanisms for brain recovery. The first happens early and automatically as the circulation to an area is restored, and the edema recedes. The second is termed neuroplasticity and involves neurons in the brain reorganizing their structure, function, and interconnections. While damaged neurons in the central nervous system often die and cannot regenerate, undamaged axons have been shown to grow new nerve endings to connect to other intact neurons, called neurocortical sprouting. Also, patients who had a stroke may be able to train their brains to perform tasks using previously latent functional pathways. This learning is stimulated primarily by highly repetitive practice. Researchers are investigating ways this could be augmented with medications or transcranial magnetic stimulation. The AHA/ASA found that roughly 70% of Medicare patients diagnosed with acute stroke utilize Medicare-covered post-acute care. About 32% are sent to skilled nursing facilities for rehabilitation, 22% to inpatient rehabilitation facilities (free-standing or within an acute care hospital), and 15% are discharged directly home with home health care. This data means that 30% of all patients with stroke covered by Medicare get no post-acute rehabilitation, which has increased since the 1990s (CDC, 2023c; NINDS, 2020; Winstein et al., 2016).
Before discharge, all patients who had a stroke should be screened for depression and appropriately treated if present. Additionally, a formal assessment of functional ADLs, instrumental ADLs (iADLs), communication skills, and functional mobility should be completed by a clinician with expertise in rehabilitation. If they qualify, all patients should receive early rehabilitation in an environment with organized interprofessional stroke care at an intensity commensurate with their tolerance and anticipated benefit. High-dose therapy within 24 hours of stroke should be avoided. The use of fluoxetine (Prozac or another selective serotonin reuptake inhibitor [SSRI]) during AIS rehabilitation to enhance motor recovery in the absence of confirmed depression is not yet well established (Powers et al., 2019). While fluoxetine has been shown to reduce depression in patients following ICH, it does not improve functional recovery and may increase the risk of fracture (Greenberg et al., 2022). The AHA/ASA Rehabilitation Guidelines (2016) recommend that patients post-stroke remain in an inpatient setting for their rehabilitation if they require therapy interventions from multiple disciplines (physical therapy [PT] and occupational therapy [OT] to address moderate to severe motor or sensory deficits, OT and SLT to address cognitive deficits, and SLT to address communication deficits) as well as skilled nursing care for:
- bowel or bladder impairment
- existing or increased risk for skin breakdown
- impaired bed mobility
- dependence on basic ADLs
- inability to manage medications independently
- increased risk for nutritional deficits (CDC, 2023c; NINDS, 2020; Winstein et al., 2016)
Inpatient rehabilitation candidates should also have a documented need for daily physician contact to help manage the following:
- significant or multiple medical comorbidities;
- complex rehabilitation issues such as bowel/bladder incontinence, spasticity, or orthotics
- acute illness
- pain management issues (CDC, 2023c; NINDS, 2020; Winstein et al., 2016)
A rehabilitation unit for patients post-acute stroke should consist of a comprehensive, evidence-based, and multidisciplinary program that focuses on the prevention of complications, medical management, and the rehabilitation of sensorimotor impairments, upper extremity activities, cognitive or communication deficits, and transitions of care to home or the community. It involves a sustained and coordinated effort from a team that includes the patient, the patient's family, caregiver(s) and friends, physicians, NPs, PAs, nurses, PTs, OTs, SLTs, recreational therapists, psychologists, nutritionists, social workers, and others. Communication and coordination are extremely important in these environments. A PT-guided balance training program is paramount to safety if there is poor balance, an increased risk of falls documented on the patient's PT or nursing assessments, or simply a decrease in the patient's balance confidence or a fear of falls secondary to the acute stroke. When the patient is appropriate for discharge back home, an individually tailored exercise program to gradually improve cardiovascular fitness is helpful for secondary stroke prevention (CDC, 2023c; NINDS, 2020; Winstein et al., 2016). The initiation of stretching and functional task training may be considered 24-48 hours following moderate ICH, but aggressive mobilization within 24 hours is not recommended, as mentioned above, for AIS patients. Early supported discharge may be appropriate following mild to moderate ICH. Home caregivers should receive practical support, psychosocial education, and training to improve balance, activity level, and overall QOL (Greenberg et al., 2022).
A meta-review of 13 systematic reviews found that when self-care was included as a component of a rehabilitation program post-stroke, it resulted in short-term (less than one year) improvements in ADLs and decreased the risk of dependence and death. A separate meta-analysis of six trials of self-care programs found that this intervention increases the quality of life and self-efficacy after stroke (Riegel et al., 2017). Other complementary treatments, such as acupuncture, are also being tested. A meta-analysis of eight randomized controlled trials was completed, including 399 patients with post-stroke spasticity treated with acupuncture versus sham procedures in one study and acupuncture plus PT versus PT alone in the other seven studies. The analysis shows no statistically significant effect on clinical outcomes (as tested by the modified Ashworth Scale [mAS]) or physiologic outcomes (as tested by the H-reflex/M-response ratio) except in two trials, which were able to show a significant improvement after the first visit only (Park et al., 2014).
Dysphagia is another common chronic sequela of stroke. A systematic review of 58 studies involving over 6,000 patients who underwent acupuncture treatment for their dysphagia showed that the acupuncture group was superior to the control with moderate heterogeneity, and the efficacy rate of acupuncture was three times that of the control group with no heterogeneity (Ye et al., 2017). In 2022, Birch and Robinson examined international clinical practice guidelines for acupuncture in post-stroke treatment. They found that across 27 countries, 84 clinical practice guidelines were written that included post-stroke care. Of the 84, 49 made statements about acupuncture, with 15 of them including positive recommendations about acupuncture for stroke rehabilitation dysphagia, motor recovery, spasticity, post-stroke pain, shoulder pain, walking, balance, upper limb extremity impairment, cognitive disorder, sleep problems, central post-stroke pain, and depression. Given that many guidelines do not address the role of acupuncture in post-stroke care, Birch and Robinson (2022) recommend that healthcare providers evaluate the current evidence before deciding on use.
Technology is also playing a role in increasing availability and decreasing the cost of post-stroke care and rehabilitation services. When stroke patients with chronic aphasia are treated with constraint-induced aphasia therapy (CIAT, also known as intensive language action therapy or ILAT), even in a computer-based format in their home, it may improve communication skills. Computer software can be personalized to an individual patient's needs, and with the development of better speech recognition software to help with word choice and pronunciation, speech therapy patients can be initially trained and then tracked remotely. Exercises can then be adjusted as the patient improves. This happens as the patient practices and works at home instead of traveling for speech therapy appointments (Palmer, 2015). In a recent systematic review, Wang and colleagues (2020) evaluated the effects of CIAT on patients with aphasia. The researchers included 12 randomized controlled trials and found that CIAT efficiently improved language performance (i.e., comprehension, repetition, and oral and written language). Wang and colleagues concluded that CIAT therapy should occur for two to three hours daily (2020).
If the patient has chronic residual deficits, many find that even after the acute phase, they may still benefit from therapies months or years later. Repetitive facilitative exercises (REFs) are a form of movement therapy to help patients recover from hemiparesis after a stroke. In one study, a combination treatment of four weeks of RFEs and orthotics was tested within a physical therapy office on 27 patients that were at least five months and an average of 35 months post-stroke. While this was a small sample size, all measures showed significant improvement after treatment. RFEs combine high repetition rate and neurofacilitation, where trained therapists use muscle spindle stretching and skin-generated reflexes to help the patient activate and move an affected limb (Tomioka et al., 2017). More recently, a randomized controlled trial was conducted to examine the combined effect of an REF program with botulinum toxin type A (BoNT-A) injection to reduce spasticity. The intervention group received RFE combined with BoNT-A, while the control received RFE only. The researchers found that the combination of RFE and BoNT-A significantly increased the efficiency of motor learning and showed promise to lessen the impairment in patients with residual stroke effects (Hokazono et al., 2022).
References
Albers, G. W., Marks, M. P., Kemp, S., Christensen, S., Tsai, J. P., Ortega-Gutierrez, S., McTaggart, R. A., Torbey, M. T., Kim-Tenser, M., Leslie-Mazwi, T., Sarraj, A, Kasner, S. E., Ansari, S. A., Yeatts, S. D., Hamilton, S., Mlynash, M., Heit, J. J., Zaharchuk, G., Kim, S., Carrozzella, J., … Lansberg, M. G., (2018). Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. The New England Journal of Medicine, 378, https://doi.org/10.1056/NEJMoa1713973
Birch, S., & Robinson, N. (2022). Acupuncture as a post-stroke treatment option: A narrative review of clinical guideline recommendations. Phytomedicine, 104, 154297. https://doi.org/10.1016/j.phymed.2022.154297
Caplan, L. R. (2022). Stroke: Etiology, classification, and epidemiology. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/stroke-etiology-classification-and-epidemiology
Centers for Disease Control and Prevention. (n.d.) Interactive atlas of heart disease and stroke. Retrieved on May 15, 2023, from https://nccd.cdc.gov/DHDSPAtlas/Default.aspx
Centers for Disease Control and Prevention. (2022a). About stroke: Stroke signs and symptoms. https://www.cdc.gov/stroke/signs_symptoms.htm
Centers for Disease Control and Prevention. (2022b). Prevent stroke: What you can do. https://www.cdc.gov/stroke/prevention.htm
Centers for Disease Control and Prevention. (2023a). Know your risk for stroke. https://www.cdc.gov/stroke/risk_factors.htm
Centers for Disease Control and Prevention. (2023b). Stroke facts. https://www.cdc.gov/stroke/facts.htm
Centers for Disease Control and Prevention. (2023c). Treat and recover from stroke. https://www.cdc.gov/stroke/treatments.htm
Chong, J. Y. (2022a). Intracranial hemorrhage. Merck Manual Professional Version. https://www.merckmanuals.com/professional/neurologic-disorders/stroke/intracerebral-hemorrhage
Chong, J. Y. (2022b). Ischemic stroke. Merck Manual Professional Version. https://www.merckmanuals.com/professional/neurologic-disorders/stroke/ischemic-stroke
Chong, J. Y. (2022c). Overview of stroke. Merck Manual Professional Version. https://www.merckmanuals.com/professional/neurologic-disorders/stroke/overview-of-stroke
Chong, J. Y. (2022d). Transient ischemic attack (TIA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/neurologic-disorders/stroke/transient-ischemic-attack-tia
Dong, J., Wang, F., & Sundararajan, S. (2020). Use of dual antiplatelet therapy following ischemic stroke. Stroke, 51(5), e78–e80. https://doi.org/10.1161/STROKEAHA.119.028400
Franco, J. (2018). Imaging and treatment of strokes. Radiologic Technology, 89(6), 549-568. https://pubmed.ncbi.nlm.nih.gov/30420526
Goldstein, L. B. (2023). Use and utility of stroke scales and grading systems. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/use-and-utility-of-stroke-scales-and-grading-systems
Greenberg, S. M., Ziai, W. C., Cordonnier, C., Dowlatshahi, D., Francis, B., Goldstein, J. N., Hemphill, J. C., III., Johnson, R., Keigher, K. M., Mack, W. J., Mocco, J., Newton, E. J., Ruff, I. M., Sansing, L. H., Schulman, S., Selim, M. H., Sheth, K. N., Spring, N., Sunnerhagen, K. S., & on behalf of the American Heart Association/American Stroke Association. (2022). 2022 guideline for the management of patients with spontaneous Intracerebral hemorrhage: A guideline from the American Heart Association/American Stroke Association. Stroke, 53(7), e282-e361. https://doi.org/10.1161/STR.0000000000000407
Hennekens, C. H. (2022). Overview of primary prevention of cardiovascular disease. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/overview-of-primary-prevention-of-cardiovascular-disease
Hokazono, A., Etoh, S., Jonoshita, Y., Kawahira, K., Shimodozono, M. (2022). Combination therapy with repetitive facilitative exercise program and botulinum toxin type A to improve motor function for the upper-limb spastic paresis in chronic strokes: A randomized controlled trial. Journal of Hand Therapy, 35(4), 507-515. https://doi.org/10.1016/j.jht.2021.01.005
Hui, C., Tadi, P., & Patti, L. (2022). Ischemic stroke. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK499997
The Joint Commission. (n.d.). Advanced stroke certification. Retrieved June 5, 2023, from https://www.jointcommission.org/what-we-offer/certification/certifications-by-setting/hospital-certifications/stroke-certification/advanced-stroke
The Joint Commission. (2023). Electronic clinical quality measures. https://www.jointcommission.org/measurement/specification-manuals/electronic-clinical-quality-measures
Kleindorfer, D. O., Towfighi, A., Chaturvedi, S., Cockroft, K. M., Gutierrez, J., Lombardi-Hill, D., Kamel, H., Kernan, W. N., Kittner, S. J., Leira, E. C., Lennon, O., Meschia, J. F., Nguyen, T. N., Pollak, P. M., Santangeli, P., Sharrief, A. Z., Smith, S. C. Jr., Turan, T. N., & Williams, L. S. (2021). Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7), e364-e467. https://doi.org/10.1161/STR.0000000000000375
Meng, R., Ding, Y., Asmaro, K., Brogan, D., Meng, L., Sui, M., Shi, J., Duan, Y., Sun, Z., Yu, Y., Jia, J., & Ji, X. (2015). Ischemic conditioning is safe and effective for octo- and nonagenarians in stroke prevention and treatment. Neurotherapeutics: The Journal of the American Society for Experimental NeuroTherapeutics, 12(3), 667-77. https://doi.org/10.1007/s13311-015-0358-6
Meschia, J. F., Bushnell, C., Boden-Albala, B., Braun, L. T., Bravata, D. M., Chaturvedi, S., Creager, M. A., Eckel, R. H., Elkind, M. S. V., Fornage, M., Goldstein, L. B., Greenberg, S. M., Horvath, S. E., Iadecola, C., Juach, E. C., Moore, W. S., & Wilson, J. A. (2014). Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 45(12), 3754-3832. https://doi.org/10.1161/STR.0000000000000046
National Heart, Lung, and Blood Institute. (2013a). Hemorrhagic stroke [Image]. https://commons.wikimedia.org/wiki/File:Stroke_hemorrhagic.jpg
National Heart, Lung, and Blood Institute. (2013b). Ischemic stroke [Image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Stroke_ischemic.jpg
National Heart, Lung, and Blood Institute. (2022a). Stroke symptoms. https://www.nhlbi.nih.gov/health/stroke/symptoms
National Heart, Lung, and Blood Institute. (2022b). What is a stroke? https://www.nhlbi.nih.gov/health-topics/stroke
National Institutes of Health. (2010). Cerebral aneurysm [Image]. Wikimedia. https://commons.wikimedia.org/wiki/File:Cerebral_aneurysm_NIH.jpg
National Institute of Neurological Disorders and Stroke (2020). Post-stroke rehabilitation. https://catalog.ninds.nih.gov/publications/post-stroke-rehabilitation
National Institute of Neurological Disorders and Stroke (2023a). Shareable resources: Infographics. https://www.stroke.nih.gov/materials/infographics.htm
National Institute of Neurological Disorders and Stroke. (2023b). Cerebral aneurysms. https://www.ninds.nih.gov/health-information/disorders/cerebral-aneurysms
Nikoubashman, O., Schürmann, K., Othman, A. E., Bach, J-P., Wiesmann, M., & Reich, A. (2018). Improvement of endovascular stroke treatment: A 24-hour neuroradiological on-site service is not enough. BioMed Research International, 2018, 1-8. https://doi.org/10.1155/2018/9548743
Nogueira, R. G., Jadhav, A. P., Haussen, D. C., Bonafe, A. Budzik, R. F., Bhuva, P., Yavagal, D. R., Ribo, M., Cognard, C., Hanel, R. A., Sila, C. A., Hassan, A. E., Millan, M., Levy, E. I., Mitchell, P., Chen, M., English, J. D., Shah, Q. A., Silver, F. L., Pereira, V. M.,… Jovin, T. G. (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. The New England Journal of Medicine, 378, 11-21. https://doi.org/10.1056/NEJMoa1706442
Oliveira-Filho, J., & Lansberg, M. G. (2023). Neuroimaging of acute stroke. UpToDate. Retrieved June 5, 2023, https://www.uptodate.com/contents/neuroimaging-of-acute-stroke
Oliveira-Filho, J. & Mullen, M. T. (2023). Initial assessment and management of acute stroke. UpToDate. Retrieved June 5, 2023, from https://www.uptodate.com/contents/initial-assessment-and-management-of-acute-stroke
Palmer, R. (2015). Innovations in aphasia treatment after stroke: Technology to the rescue. British Journal of Neuroscience Nursing, 11(2), 38-42. https://doi.org/10.12968/bjnn.2015.11.Sup2.38
Park, S. W., Yi, S. H., Lee, J. A., Hwang, P. W., Yoo, H. C., & Kang, K. S. (2014). Acupuncture for the treatment of spasticity after stroke: A meta-analysis of randomized controlled trials. Journal of Alternative and Complementary Medicine, 20(9), 672-82. https://doi.org/10.1089/acm.2014.0097
Powers, W. J., Rabinstein, A. A., Ackerson, T., Adeoye, O. M., Bambakidis, N. C., Becker, K., Biller, J., Brown, M., Demaerschalk, B. M., Hoh, B., Jauch, E. C., Kidwell, C. S., Leslie-Mazwi, T. M., Ovbiagele, B., Scott, P. A., Sheth, K. N., Southerland, A. M., Summers, D. V., Tirschwell, D. L., and on behalf of the American Heart Association Stroke Council. (2019). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 50(12), e344-e418. https://doi.org/10.1161/STR.0000000000000211
Riegel, B., Moser, D. K., Buck, H. G., Dickson, V. V., Dunbar, S. B., Lee, C. S., Lennie, T. A., Lindenfeld, J., Mitchell, J. E., Treat-Jackson, D. J., & Webber, D. E. (2017). Self-care for the prevention and management of cardiovascular disease and stroke: A scientific statement for healthcare professionals from the American Heart Association. Journal of the American Heart Association, 6(9), e006997. https://doi.org/10.1161/JAHA.117.006997
Rordorf, G., & McDonald, C. (2023). Spontaneous Intracranial hemorrhage: Acute treatment and prognosis. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/spontaneous-intracerebral-hemorrhage-acute-treatment-and-prognosis
Rost, N. S., & Simpkins, A. (2023). Overview of secondary prevention of ischemic stroke. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/overview-of-secondary-prevention-of-ischemic-stroke
Saver, J. L., Chaisinanunkul, N., Campbell, B. C. V., Grotta, J. C., Hill, M. D., Khatri, P., Landen, J., Lansberg, M. G., Venkatasubramanian, C., Albers, G. W., & XIth Stroke Treatment Academic Industry Roundtable. (2021). Standardized nomenclature for modified Rankin Scale global disability outcomes: Consensus recommendations from stroke therapy academic industry roundtable XI. Stroke, 52(9), 3054-3062. https://doi.org/10.1161/strokeaha.121.034480
Singer, R. J., Ogilvy, C. S., & Rordorf, G. (2021). Subarachnoid hemorrhage grading scales. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/subarachnoid-hemorrhage-grading-scales
Singer, R. J., Ogilvy, C. S., & Rordorf, G. (2023). Aneurysmal subarachnoid hemorrhage: Treatment and prognosis. UpToDate. Retrieved May 16, 2023, from https://www.uptodate.com/contents/aneurysmal-subarachnoid-hemorrhage-treatment-and-prognosis
Spiotta, A. M., Chaudry, M. I., Hui, F. K., Turner, R. D., Kellogg, R. T. & Turk, A. S. (2015). Evolution of thrombectomy approaches and devices for acute stroke: A technical review. Journal of NeuroInterventional Surgery, 7, 2–7. https://doi.org/10.1136/neurintsurg-2013-011022
Tadi, P., & Lui, F. (2023). Acute stroke. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK535369
Tomioka, K., Matsumoto, S., Ikeda, K., Uema, T., Sameshima, J. I., Sakashita, Y., Kaji, T., & Shimodozono, M. (2017). Short-term effects of physiotherapy combining repetitive facilitation exercises and orthotic treatment in chronic post-stroke patients. Journal of Physical Therapy Science, 29(2), 212-215. https://doi.org/10.1589/jpts.29.212
Tsao, C. W., Aday, A. W., Almarzooq, Z. I., Anderson, C. A. M., Arora, P., Avery, C. L., Baker-Smith, C. M., Beaton, A. Z., Boehme, A. K., Buxton, A. E., Commodore-Mesah, Y., Elkind, M. S. V., Everson, K. R., Eze-Nliam, C., Fugar, S., Generoso, G., Heard, D. G., Hiremath, S., Ho, J. E., Kalani, R., . . . American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Committee (2023). Heart disease and stroke statistics—2023 Update: A report from the American Heart Association. Circulation,147(8), e93–e621. https://doi.org/10.1161/CIR.0000000000001123
Unnithan, A. K. A., Das, J. M., & Mehta, P. (2022). Hemorrhagic stroke. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK559173
Waldman, A., Tadi, P., & Rawal, A. R. (2022). Stroke center certification. StatPearls [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK535392
Wändell, P., Carlsson, A. C., Holzmann, M., Ärnlöv, J., Johansson, S. E., Sundquist, J., & Sundquist, K. (2017). Association between antithrombotic treatment and hemorrhagic stroke in patients with atrial fibrillation-a cohort study in primary care. European Journal of Clinical Pharmacology, 73(2), 215-221. https://doi.org/10.1007/s00228-016-2152-8
Wang, G., Ge, L., Zheng, Q., Huang, P., & Xiang, J. (2020). Constraint-induced aphasia therapy for patients with aphasia: A systematic review. International Journal of Nursing Sciences, 28(7), 349-358. https://doi.org/10.1016/j.ijnss.2020.05.005
Winstein, C. J., Stein, J., Arena, R., Bates, B., Cherney, L. R., Cramer, S. C., Deruyter, F., Eng, J. J., Fisher, B., Harvey, R. L., Lang, C. E., MacKay-Lyons, M., Ottenbacher, K. J., Pugh, S., Reeves, M. J., Richards, L. G., Stiers, W., & Zorowitz, R.D. (2016). Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 47, e98–e169. https://doi.org/10.1161/STR.0000000000000098
World Health Organization. (2021). Cardiovascular diseases (CVDs). https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Yaghi, S., Willey, J. Z., Cucchiara, B., Goldstein, J. N., Gonzales, N. R., Khatri, P., Kim, L. J., Mayer, S. A., Sheth, K. N., & Schwamm, L. H. (2017). Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke, 48, e343–e361. https://doi.org/10.1161/STR.0000000000000152
Ye, Q., Xie, Y., Shi, J., Xu, Z., Ou, A., & Xu, N. (2017). Systematic review on acupuncture for treatment of dysphagia after stroke. Evidence-based Complementary and Alternative Medicine: eCAM, 2017, 6421852. https://doi.org/10.1155/2017/6421852
Zhao, W., Li, S., Ren, C., Meng, R., Jin, K., & Ji, X. (2019). Remote ischemic conditioning for stroke: Clinical data, challenges, and future directions. Annals of Clinical and Translational Neurology, 15(6), 186-196. https://doi.org/10.1002/acn3.691