About this course:
This course reviews the risks, symptoms, complications, and treatment for various foodborne diseases. Specifically, this course will focus on the foodborne diseases reportable to the Centers for Disease Control and Prevention (CDC), including foodborne botulism, infant botulism, brucellosis, campylobacteriosis, cryptosporidiosis, cyclosporiasis, acute hepatitis A, listeriosis, salmonellosis, Escherichia coli, trichinellosis, tularemia, and vibriosis, as well as non-infectious foodborne diseases including mercury poisoning, arsenic poisoning, and scombroid syndrome.
Course preview
This course reviews the risks, symptoms, complications, and treatment for various foodborne diseases. Specifically, this course will focus on the foodborne diseases reportable to the Centers for Disease Control and Prevention (CDC), including foodborne botulism, infant botulism, brucellosis, campylobacteriosis, cryptosporidiosis, cyclosporiasis, acute hepatitis A, listeriosis, salmonellosis, Escherichia coli, trichinellosis, tularemia, and vibriosis, as well as non-infectious foodborne diseases including mercury poisoning, arsenic poisoning, and scombroid syndrome.
Upon completion of this activity, learners should be able to:
- describe the epidemiologic resources and measures used in the US for outbreaks of foodborne diseases, including reportable foodborne diseases
- describe common physiologic changes caused by infectious foodborne disease and implications for groups at increased risk of occurrence and severity
- discuss the specific medical tests and samples required for the diagnosis of various foodborne diseases
- differentiate among infectious foodborne diseases in the US that are commonly experienced, those that require hospitalization, and those with a significant risk of mortality
- identify the onset, course, symptoms, complications, treatment, and food sources for common foodborne diseases
- discuss examples and health risks of non-infectious foodborne diseases, including mercury poisoning, arsenic poisoning, and scombroid poisoning
- evaluate the implementation of general food safety practices in the home and measures specific to severe and common foodborne diseases
How many people inspect cans in the grocery store for bulging ends? Concern over botulism in canned foods that began in 1919, mainly olives and green beans, impacts what some people do a century later. At that time, sensational journalism claimed, "one drop . . . would depopulate the Earth." In the commercial canning industry, voluntary and governmental changes improved food safety. It is a reminder that knowledge and actions are necessary to keep the food supply safe and involve individuals and public health leaders in the surveillance and regulation of foodborne illnesses (Kazanjian, 2018).
Epidemiologic Resources in the US for Foodborne Disease
According to the Centers for Disease Control and Prevention (CDC), there are 250 foodborne diseases. Bacteria, viruses, and parasites cause many foodborne infections, but toxins and chemicals in food can also cause disease. The US's five most common foodborne disease agents are Norovirus (NoV), Salmonella, Clostridium perfringens, Campylobacter, and Staphylococcus aureus. The microorganisms most likely to result in hospitalization are Clostridium botulinum, Listeria monocytogenes, Escherichia coli (E. coli), and Vibrio. The CDC estimates that 48 million people get sick, 128,000 are hospitalized, and 3,000 die annually from foodborne diseases. Foodborne disease affects approximately 1 in every 6 people yearly. A standard used to determine the impact of foodborne pathogens is the disability-adjusted life year (DALY). DALY combines loss of life and decreased health because of illness compared with an ideal state of health, using time as the standard measure (CDC, 2019b, 2020a; Gotfried, 2021a; O'Brien, 2017).
Nurses are responsible for promoting access to current information for patients who are at risk for or experiencing foodborne disease. The CDC is the governmental agency responsible for surveillance, investigations, and protocols for preventing, identifying, and eradicating foodborne disease outbreaks. Case reporting to the CDC is voluntary for most diseases if a single location is involved. Reporting occurs through the National Outbreak Reporting System. State health departments may also provide specific deoxyribonucleic acid (DNA) identification, especially for Salmonella, Shigella, Listeria, and Shiga toxin-producing E. coli (STEC). Other resources for foodborne disease reporting include OutbreakNet Enhanced, which assists state health departments during outbreaks and identifies gaps in investigations; FoodCORE, with regional locations for response to outbreaks; and the Integrated Food Safety Centers of Excellence, which provides training and information to state and local health departments within regions and through university partners in Colorado, Florida, Minnesota, New York, Oregon, and Tennessee (CDC, 2018b). The Food and Drug Administration (FDA, 2018a) monitors foodborne organisms from any food product—agricultural or commercial—regulated by governmental standards.
When two or more people get the same illness from the same contaminated food or drink, it is determined to be an outbreak by the CDC. The agency maintains records on multistate outbreaks. Examples of multistate outbreaks in 2021 are as follows:
- Salmonella: salami sticks, seafood, onions, Italian-style meats, pre-packaged salads, frozen cooked shrimp, raw frozen breaded stuffed chicken products, cashew brie, and ground turkey
- E. coli: packaged salads, baby spinach, and cake mix
- Listeria monocytogenes: fresh express packaged salads, Dole packaged salads, fully cooked chicken, and queso fresco (CDC, 2022c)
Figure 1 from the CDC outlines the steps to manage a foodborne disease outbreak.
Figure 1
CDC Outbreak Investigation Process

(CDC, 2018d)
General Symptoms of Foodborne Disease
Gastroenteritis refers to the symptoms of any disease affecting the gastrointestinal tract. Infectious foodborne diseases are the most common cause of gastroenteritis. Primary symptoms are diarrhea and vomiting. Diarrhea is defined as three or more loose or liquid stools a day. Acute diarrhea lasts less than 14 days, while chronic diarrhea lasts more than 14 days. Prolonged or frequent vomiting can deplete intravascular fluid, causing tachycardia and hypotension. In addition, the acid-base balance is affected, with vomiting more likely to result in metabolic alkalosis and diarrhea more commonly resulting in metabolic acidosis. Both vomiting and diarrhea can cause hypokalemia. Depending on the etiology of the foodborne disease, the degree and severity of vomiting and diarrhea can vary. Therefore, nurses should teach patients to recognize which symptoms can be managed with home treatment and which require medical treatment (Gotfried, 2021a; Hinkle et al., 2022).
Foodborne diseases are usually acute illnesses that last less than a week. Many people do not seek treatment. A challenge with foodborne diseases is that healthcare providers (HCPs) do not see many of those affected. Sometimes, patients do not seek treatment for days after infection. The most common symptoms are the sudden onset of diarrhea, nausea, vomiting, abdominal cramping, and fever. Symptoms that indicate a need for medical intervention include bloody stools, a high fever (over 102°F), prolonged vomiting or an inability to keep liquids down, diarrhea for more than 3 days, and severe dehydration with decreased urination or postural hypotension. The most common acute complication is dehydration. Additional risks accompany any foodborne illness that occurs during pregnancy, resulting in miscarriage or stillbirth. Long-term complications can include chronic arthritis, hemolytic uremic syndrome, and brain or nerve damage (CDC, 2022b; National Institute
...purchase below to continue the course
Risk Factors for Foodborne Disease and Complications
Foodborne diseases can affect anyone; however, children younger than 5, adults over 65, and immunocompromised and pregnant individuals are at increased risk. Those at the most significant risk from gastrointestinal infections are young children. Dehydration from diarrhea and vomiting is the immediate physiologic challenge, but the infection may also damage the gut, resulting in nutritional and developmental deficiencies. Young children with Salmonella are three times more likely to be hospitalized. In children under 5 with E. coli 0157 infections, 1 in 7 will develop kidney failure. Worldwide, gastroenteritis currently results in the death of approximately 1.5 million children annually. While much credit is given to improved water sanitation, oral rehydration for infants has also improved outcomes. Rotavirus, the most common viral foodborne infection among children, has decreased in incidence in the US by 80% since the implementation of routine immunization in 2006 (Gotfried, 2021a).
People over 65 are also at higher risk due to decreased immunity. Hospitalization is necessary for approximately half of people over 65 with Salmonella, Campylobacter, Listeria, or E. coli. Older patients are more likely to have cardiac compromise or renal insufficiency, which increases the risk for fluid and electrolyte imbalance exacerbated by infectious disease. The risk for aspiration from vomiting increases in older adults with a decreased level of consciousness. Antiemetics with central nervous system (CNS) side effects present additional risks to older adults. Use the lowest effective dose of antiemetics for older patients, as the risks of falls increases due to dehydration, hypotension, and dizziness. Nurses should be cautious with aggressive fluid volume replacement for older adults. For example, using hypotonic fluids in replacement therapy can provoke hyponatremia. The immunocompromised state of patients with diabetes, liver disease, kidney disease, HIV/AIDS, alcoholism, and cancer also increases the risk for and severity of foodborne diseases. For example, people on dialysis are 50 times more likely to get infected with Listeria. Pregnant individuals are also at increased risk of foodborne disease and are 10 times more likely to get a Listeria infection (CDC, 2019a; Gotfried, 2021a; Hinkle et al., 2022).
Diagnostic Testing for Foodborne Disease
The classic diagnostic testing for foodborne disease with gastroenteritis is stool cultures. A stool culture is not routinely performed but is indicated by diarrhea for more than 3 days, in the presence of a high fever, or with severe illness. The stool may also be examined for blood, mucus, white blood cells (WBCs), parasites, or specific toxins. If diarrhea lasts more than 2 weeks, the stool may also be examined for ova and parasites. Subacute, chronic watery diarrhea indicates a need for parasitic testing. Acute diarrhea with gross blood requires a stool culture for E. coli 0157:H7. This test needs a specific order since it is not part of a standard stool culture. Other indications for stool testing include immunosuppression, exposure to a known outbreak, recent travel, or recent antibiotic use. Polymerase chain reaction (PCR) testing of stool can detect subtypes of organisms and is especially useful for E. coli subtypes. This rapid diagnostic testing (RDT) of stool identifies up to 22 common pathogens—which include bacteria, viruses, and parasites—within an hour of sample preparation. While this testing is expensive, it may reduce the total number of tests a patient must undergo and allow the appropriate medication treatment to begin earlier. Diagnostic stewardship in using RDT necessitates a thorough history and review of symptoms by HCPs to ensure symptoms of infectious diarrhea are present (Gotfried, 2021a; Hinkle et al., 2022; Qasmieh et al., 2018).
Other diagnostic tests for foodborne diseases include serum testing for blood urea nitrogen (BUN), creatinine, electrolytes, and acid-base evaluation. A complete blood count (CBC) is usually non-specific, but parasitic infections demonstrate eosinophilia. Renal function tests and a CBC should be initiated for patients with foodborne diseases with the risk of hemolytic-uremic syndrome. With E. coli 0157:H7, where onset begins early, renal testing should begin one week after the onset of symptoms. Another test specific to E. coli 0157:H7 is a rapid enzyme assay for detecting Shiga toxin in the stool. This potent toxin produced by bacteria breaks down tissues, especially in the kidneys. WBCs in the stool is more common with enteric pathogens, including Salmonella, Shigella, Campylobacter, and E. coli, and diarrhea does not usually contain gross blood. A sigmoidoscopy with culture and biopsy is indicated for adults with grossly bloody diarrhea to evaluate for mucosal changes that can differentiate between amebic dysentery, shigellosis, or E. coli 0157:H7 (Gotfried, 2021a; Hinkle et al., 2022).
Another tool in investigating foodborne disease outbreaks is strain typing. Traditionally, this involved a pulse-field gel electrophoresis (PFGE) procedure. However, newer techniques called matrix-assisted laser desorption/ionization-time of flight mass-spectrometry and whole-genome sequencing have improved this process. Whole-genome sequencing has only recently become rapid and affordable. While these tools are helpful during outbreaks, challenges include few qualified personnel and complicated cost reimbursement (Lee, 2017).
The spread of foodborne diseases is also possible in hospital settings as part of diagnostic testing. For example, nosocomial Salmonella infections occurred with inadequate decontamination of an endoscope after endoscopic retrograde cholangiopancreatography. Adequate training and familiarity with the specific equipment used are essential to prevent similar transmissions of organisms (Robertson et al., 2017).
Infectious Foodborne Diseases in the US
The CDC ranks the most common foodborne illnesses annually (see Table 1). In this report, infectious foodborne diseases are initially ordered by their occurrence, hospitalization rates, and mortality rates and then described. The CDC identifies the top five diseases in each category. The rest of the report describes other foodborne diseases, differentiated first by reportability and then by either occurrence or risk. Finally, non-reportable diseases are grouped by causative organisms: bacteria, viruses, and parasites (CDC, 2018a).
Table 1
The Leading Foodborne Pathogens in the US
Top 5 pathogens contributing to domestically acquired foodborne illnesses
| Top 5 pathogens contributing to domestically acquired foodborne illnesses resulting in hospitalization | Top 5 pathogens contributing to domestically acquired foodborne illnesses resulting in death |
|
|
|
(CDC, 2018a)
Norovirus
The most common foodborne disease in the US and globally is NoV. Current CDC reports estimate 20.8 million cases annually with 56,000 hospitalizations and 149 deaths. The latest global data from the World Health Organization (WHO) reported 125 million cases and 35,000 deaths attributed to NoV infections. This viral infection spreads predominately by human feces and vomit. Environmental contamination by virus particles can last from several days to months. NoV is highly infectious, and neither future protection nor cross-protection from other genotypes occurs. Susceptibility to NoV infection and disease is related to histo-blood group antigen (HBGA) expression, as NoV binds to HBGAs. NoV can bind to animal cells, especially oyster guts, and an NoV-like particle that binds to HBGA-like carbohydrates in the cell wall of lettuce have been identified. Infected food handlers, both symptomatic and asymptomatic, have served as sources. The current recommendation is handwashing with soap and water since alcohol-based hand sanitizer is not as effective in eliminating NoV. An estimated 14% of NoV infections result from ingesting contaminated food. NoV binding to bacteria occurs in the human microbiome and foods, protecting the NoV during food processing treatments. Viruses like NoV usually affect the villi of the small bowel and push more fluid and electrolytes into the bowel lumen (transudation), causing watery diarrhea. The predominant symptom of NoV in adults is diarrhea, while vomiting is more common in children. Fevers can occur, and patients may also report abdominal cramping, headaches, and muscle pain (CDC, 2018a, 2019b; Gotfried, 2021a).
Salmonella (Non-Typhoidal)
Salmonella causes non-typhoidal and typhoid fever. Salmonella (non-typhoidal) prompts approximately 1.35 million illnesses, 19,000 hospitalizations, and 420 deaths in the US annually. Salmonella enterica serotype Typhi (typhoid fever) causes an estimated 5,700 illnesses, of which 1,600 are acquired in the US, with 600 cases requiring hospitalization but no deaths recorded. The incidence of Salmonella increases in the summer months. Children under 5, non-breastfed infants, adults over 65, people who are immunocompromised, and those who take certain medications (e.g., that reduce stomach acid) are more at risk (CDC, 2019b, 2022d). The Netherlands experienced the most significant single-country foodborne outbreak worldwide, with laboratory confirmation of 1,149 cases of Salmonella in 2012 from smoked salmon (Suijkerbuijk et al., 2016).
Non-typhoidal salmonellosis has a mortality rate below 1% but is highly infective, with a single bacteria of some strains sufficient to initiate disease. The onset of symptoms begins 6 to 72 hours after exposure, and acute symptoms usually last 1 to 2 days. Symptoms resolve after 4 to 7 days, but the dose and strain may alter severity and duration. The organism can shed in the stool for several weeks after infection. Typical symptoms include nausea, vomiting, abdominal cramps, diarrhea, fevers, and headaches. Complications often occur in high-risk groups with a significant risk for dehydration and electrolyte balance. Sequelae include reactive arthritis, an autoimmune disorder occurring 3 to 4 weeks after infection, and septicemia or bacteremia that affects other internal organs and tissues. Extra-intestinal, invasive Salmonella infection can affect the bone (osteomyelitis), joints (septic arthritis), brain, and nervous system (meningitis). Antibiotics are not generally used in treatment but are indicated for severe illnesses or high-risk patients (CDC, 2019b, 2022d; FDA, 2012).
Typhoid fever, caused by S. typhi and S. paratyphi, has a mortality rate of 10% if left untreated. These species of Salmonella are only found in human hosts; thus, foods contaminated with human feces are the primary risk factor. Fewer than 1,000 cells are needed to cause infection. The onset is usually within 1 to 3 weeks but may be as long as 2 months after exposure. Symptoms include a high fever (103–104°F), lethargy, abdominal pain, diarrhea or constipation, headaches, general aching pain, anorexia, and occasionally, a flat, rose-colored, spotty rash. Complications include septicemia, which can lead to endocarditis, septic arthritis, or chronic gallbladder infection. Chronic infection of the gallbladder can make a person become a carrier. Intestinal perforation, neurologic involvement, and death can result from systemic infection (CDC, 2022e; FDA, 2012).
Both types of Salmonella can be foodborne but also spread via fecal particles or contaminated water. Traditionally, Salmonella is associated with meat, especially chicken. Currently, more cases are attributed to fresh produce; even dry foods, such as spices, have led to outbreaks. The list of linked foods is extensive, including eggs, dairy products, yeast, coconut, cake mixes, cream-filled desserts, dried gelatin, peanut butter, cantaloupes, tomatoes, and chocolate. While food testing includes rapid antibody and molecular-based assays, the presence of Salmonella in the culture is currently required to meet regulatory standards for confirmation (CDC, 2022e; FDA, 2012).
Clostridium Perfringens
Non-pathogenic Clostridium perfringens is common in the environment and the human digestive system. Clostridium perfringens replicates quickly and, once in the small intestine, begins to make an enterotoxin. C. perfringens type A contains the carboxypeptidase-E (CPE) gene that causes food poisoning from the toxin. Less frequently, types B, C, D, and E contain the CPE gene. The CPE gene works mainly in the small intestine by activating proteins with the release of enterotoxins, increasing fluid and electrolyte losses. Clostridium perfringens in food usually results in abdominal cramps and mild self-limiting diarrhea. Symptom onset is typically 6 to 24 hours after eating the contaminated food. Patients rarely have vomiting or fevers. Resolution usually occurs within 24 hours. Hospitalization is rarely required and rarely fatal. In some cases, watery diarrhea can cause significant fluid loss and electrolyte imbalance, with a risk for cardiac dysrhythmias. Another concern is damage to the small bowel with a risk of perforation, which can be fatal (Bush & Vazquez-Perteho, 2021a; FDA, 2012).
A second foodborne disorder from C. perfringens, enteritis necroticans (Pig-bel form), occurs internationally but is rare in the US. It is more severe and often fatal. Along with abdominal pain, vomiting, and diarrhea, affected patients may experience abdominal distention, gassy bloating, and bloody diarrhea. The organism produces a beta toxin that causes bowel necrosis. The beta toxin is trypsin-sensitive, and adequate levels of trypsin contribute to the disease's resolution. Sweet potatoes inhibit trypsin, and a large intake is not recommended (FDA, 2012).
Meat is the most common food source for C. perfringens. The bacteria can withstand temperatures up to 140°F. Prompt refrigeration of leftover cooked meat and reheating to an internal temperature of 170°F are recommended. Fish have various genotypes of C. perfringens, including type A; these are found predominately on the external surface, indicating environmental contamination and increasing consumer risks (Sabry et al., 2016). Therefore, commercial food preparation is more commonly the source rather than the home. Treatment is supportive, and antibiotics are not given (Bush & Vazquez-Pertejo, 2021b; Sabry et al., 2016).
Campylobacter
Campylobacter is an organism found in both domestic animals and fowl. Sources of infection include contact with infected animals (frequently puppies) or ingestion of contaminated food. The route of infection is either fecal-oral or sexual contact. The incidence in the US is about 845,000 annually, with a mortality rate of approximately 76 patients annually. Campylobacter infections cause 22,500 DALYs annually. The two most common species are Campylobacter jejuni and Campylobacter coli. People with comorbidities were 14 times more likely to have a hospital admission based on stool cultures. Campylobacter fetus poses a specific risk to fetuses and neonates and has a mortality rate of up to 70%. This disorder is associated with contaminated food and beverages and animal contact. The peak incidence of Campylobacter occurs during age 1 to 5 years. Adults, especially those over age 65, are more likely to be affected if they have conditions like diabetes, cirrhosis, or immunodeficiency. Meningitis can develop in infants with C. jejuni. Campylobacter affects more males than females (Bush & Vazquez-Pertejo, 2022a; CDC, 2022a; O'Brien, 2017).
Undercooked poultry is the most common source of Campylobacter, and chicken livers pose a significant risk from inadequate cooking. Other food sources include unpasteurized dairy products, vegetables, and seafood. Therefore, avoiding cross-contamination is critical, especially when working with raw poultry products (Bush & Vazquez-Pertejo, 2022a; FDA, 2012; O'Brien, 2017).
Campylobacter most frequently results in mild acute enteritis that is self-limiting but can become severe or result in colitis. Watery diarrhea is the most common symptom, but bloody diarrhea can occur. Systemic Campylobacter infection can provoke a fever of 100.4°F to 104°F, which follows a relapsing or intermittent course. The fever can accompany abdominal pain in the right lower quadrant, headaches, and myalgias. People in industrialized countries experience more severe symptoms than people in developing countries, likely due to acquired immunity in the latter group (Facciola et al., 2017). Some people can exhibit subacute bacterial endocarditis, reactive arthritis, meningitis, or fevers of unknown origin rather than enteric symptoms. Stool samples contain WBCs, and rapid molecular stool tests are used for diagnosis. Antibiotics are not prescribed routinely, as the infection normally resolves spontaneously. Erythromycin (Erythrocin) and azithromycin (Zithromax) are given when spontaneous resolution does not occur. Patients with extraintestinal infections may be prescribed gentamicin (Genoptic), ampicillin (Omnipen), erythromycin (Erythrocin), or a third-generation cephalosporin like ceftazidime (Fortaz) to prevent relapses (Bush & Vazquez-Pertejo, 2022a; CDC, 2022a; Facciola et al., 2017).
Sequelae consist of reactive arthritis, Guillain-Barre syndrome (GBS), Miller Fisher syndrome (a rare variant of GBS), hemolytic uremic syndrome, inflammatory bowel disease (IBD), and functional gastrointestinal disorders. Reactive arthritis onset is approximately 2 to 4 weeks after the infection and occurs most often in the knees; complete resolution occurs in 6 months. GBS is rare, with estimates of occurrence ranging from 1:1000 and 1:5000, but it is the most significant health consequence of Campylobacter infections. Previous Campylobacter infection has been found in approximately one-third of GBS cases worldwide. Progression is rapid, with the most significant weakness experienced in the first 2 weeks after the onset of neurologic symptoms. Approximately one-third of patients report muscle weakness for more than 3 years, and 3% have relapses of weakness for many years. Campylobacter jejuni is most closely related to the onset of GBS due to its mimicry of peripheral nerve proteins. Early diagnosis and treatment of neurologic symptoms are key to positive outcomes. Care for these patients includes plasmapheresis, high-dose immunoglobulin therapy, and supportive care with possible mechanical ventilation. Miller Fisher syndrome is a nonparalytic variation of GBS with ataxia, areflexia, and ophthalmoplegia. Hemolytic uremic syndrome following a Campylobacter infection can lead to a pulmonary-renal syndrome that causes life-threatening pulmonary hemorrhage on rare occasions. The incidence of irritable bowel syndrome (IBS) increases 3-fold following a Campylobacter infection. Other gastrointestinal disorders, such as functional dyspepsia and constipation, have been noted after infection (Facciola et al., 2017; O'Brien, 2017).
Staphylococcus Aureus
Staphylococcus aureus organisms are everywhere and virtually impossible to eliminate from the environment, as they are among the most resistant non-spore-forming human pathogens. Staphylococcus aureus survives a wide range of temperatures (44°F to 118°F, with an optimum of 95°F) and pH ranges (4.5 to 9.3, with an optimum of 7.0 to 7.5). It grows with low water activity and is highly tolerant of salts and sugars. Because of these characteristics, approximately 25% of people have Staphylococcus on their skin. Under specific conditions, like those found in food products, the organism produces a toxin that causes food poisoning. The onset of symptoms after ingestion is usually rapid, ranging from 30 minutes to 8 hours. The toxins produced are heat stable and act as pyrogenic toxin superantigens that cause immunosuppression and non-specific T-cell proliferation. The single-chain protein of this enterotoxin resists trypsin and pepsin, which usually destroy protein molecules. Each known staphylococcal enterotoxin exerts emetic activity (CDC, 2018c; FDA, 2012; Kadariya et al., 2014).
Severe vomiting begins early in the infection with accompanying nausea and abdominal stomach cramps. Diarrhea can also occur. Significant systemic symptoms from fluid loss can occur, including transient blood pressure and pulse changes, dehydration, headaches, and muscle cramping. Symptoms are intense but usually resolve in a few hours to a day. Death is rare but can occur in infants, the elderly, and those who are severely ill. Toxic identification in food and a patient's emesis or stool are diagnostic. Enzyme-linked immunosorbent assay-based (ELISA-based) methods are commonly used to identify the enterotoxin (Bush & Vasquez-Pertejo, 2021c; FDA, 2012).
The first outbreak investigation of staphylococcal foodborne disease happened in 1884 in Michigan, involving contaminated cheese. Since that time, a variety of foods have been identified, along with prevention measures. The most common foods are meat and poultry dishes (55% of S. aureus outbreaks). Handling foods increases the risk of transmission, and more cases occur in restaurants and delis compared to homes. Risk is decreased by ensuring adequate cooking time and temperature, limiting holding, and consolidating food preparation instead of taking multiple steps. Individuals can also avoid cross-contamination by adequately cleaning all processing equipment. Handwashing is key to prevention; while gloves are helpful, frequently changing gloves and handwashing are the most important measures. The first case of community-acquired methicillin-resistant Staphylococcus aureus (MRSA) occurred in a low-risk person from a food handler who had visited a nursing home and subsequently prepared coleslaw in a restaurant (Kadariya et al., 2014).
Toxoplasma Gondii
Toxoplasmosis is usually asymptomatic in healthy people, causing mild lymphadenopathy and flu-like symptoms. Pregnant and immunocompromised people, especially those with HIV/AIDS, are at the highest risk for more severe symptoms. Infection with T. gondii during pregnancy can be asymptomatic or provoke general symptoms. However, transplacental transfer to a fetus can result in increased placental thickness, fetal splenomegaly, fetal hepatomegaly, hydrocephalus, fetal ventricular dilation, fetal intracranial calcification, or fetal chorioretinitis. An ultrasound can be used to detect many of these changes. Spontaneous abortion, stillbirth, or congenital disabilities may occur. Neonates with toxoplasmosis have jaundice, a rash, hepatosplenomegaly, and a characteristic tetrad of abnormalities (i.e., bilateral retinochoroiditis, cerebral calcifications, hydrocephalus or microcephaly, and psychomotor impairment). Children born with few symptoms can still experience intellectual disability, seizure, or retinochoroiditis within months or years (Heavey, 2018; Pearson, 2020a; Pfaff & Tillett, 2016).
Serologic testing, PCR-based blood assays, cerebrospinal fluid, tissue or amniotic fluid, and histopathologic evaluation of biopsies are diagnostic. With neurologic toxoplasmosis, a head CT or MRI with contrast is performed in addition to a lumbar puncture (for patients with no signs of increased intracranial pressure). Treatment of neonates and immunocompromised patients includes pyrimethamine (Daraprim), sulfadiazine (Lantrisul), and leucovorin (Wellcovorin). Due to toxic fetal effects, these drugs are not recommended during pregnancy. Spiramycin (Provamicina) is not available in the US directly, but the FDA can assist in its acquisition. Primary prevention consists of eliminating contact with cat feces, particularly before and during pregnancy. Since soil can pose a risk for contamination, gloves should be worn for gardening. Food is commonly contaminated; strict handwashing by all food handlers and ensuring all meats reach an internal temperature of 170 °F can prevent transmission. Further research is needed, but recent studies have linked the presence of T. gondii antibodies to neurologic changes, including schizophrenia, suicidal ideation, dementia, addiction, and autism (Heavey, 2018; Pearson, 2020a; Pfaff & Tillett, 2016).
Escherichia Coli
Escherichia coli (E. coli) is among the most prevalent organisms of the normal flora within the large intestine. While the most common infection caused by E. coli affects the urinary system, some strains can lead to diarrhea and are frequently foodborne. The five strains that often cause diarrhea are enterohemorrhagic (EHEC), enterotoxigenic (ETEC), enteroinvasive, enteropathogenic (EPEC), and enteroaggregative (EAEC). ETEC most commonly causes traveler's diarrhea. Both food and water can be sources (e.g., if food is washed in local water or mishandled, initiating the infection). Symptoms are usually mild and brief, but some patients experience extremely watery stools. Antibiotics are not commonly used but can effectively reduce the duration and severity. ETEC and EPEC pose high risks for children, and EPEC frequently affects bottle-fed infants. In the past, EPEC had a high general mortality rate (25% to 50%), but improved sanitation and medical treatment of fluid loss have decreased its prevalence in developed countries. The onset of symptoms is usually within 4 hours with profuse, watery diarrhea, vomiting, and a low-grade fever. Occasionally, diarrhea lasts 21 to 120 days (Bush & Vasquez-Pertejo, 2022c; FDA, 2012; Gotfried, 2021b).
EHEC strains are associated with the most severe disease consequences, including STEC. These strains can produce cytotoxins, neurotoxins, and enterotoxins. While there are over 100 serotypes of STEC, the most common in North America is 0157:H7. These toxins harm the mucosal and vascular endothelial cells of the large intestine. Diarrhea may begin as watery but becomes grossly bloody within 24 hours. The patient often has severe abdominal pain, usually lasting from 1 to 8 days. Fevers are typically low-grade, if present, but occasionally can reach 102 °F. Hemolytic-uremic syndrome (HUS) and thrombotic thrombocytopenic purpura develop in approximately 3% to 7% of cases. A sudden decrease in hematocrit and platelets, an increase in serum creatinine, hypertension, signs of fluid overload, signs of increased bleeding events, and neurologic changes are indications of HUS. Diagnostic testing of stool cultures requires special media and a specific request for organism serotype identification. Rapid stool assay for Shiga toxin or genetic testing provides more specificity and can be essential for outbreak management (Bush & Vasquez-Pertejo, 2022d; FDA, 2012).
Most EHEC treatment is supportive. Antibiotics are not beneficial, and fluoroquinolones such as ciprofloxacin (Cipro) and levofloxacin (Levaquin) increase the risk of HUS. One possible explanation is that antibiotics break down the bacteria, releasing more of the Shiga toxin. Cattle are the primary reservoir for STEC, and changes in animal processing have reduced meat contamination. Notification of public health authorities of outbreaks of bloody diarrhea promotes greater outbreak management and prevention. Foods that have significant risks are undercooked beef (especially ground beef), unpasteurized milk, and vegetable crops contaminated by cow manure. Incidence estimates in the US for foodborne ETEC are 17,000, while other E. coli diarrhea estimates are 12,000. US-acquired STEC 0157 affects roughly 63,000 people annually, with 3,000 hospitalizations and 20 deaths. STEC non-O157 affects 169,000 people annually, with 405 hospitalizations and an estimated death rate of 0.3% (Bush & Vasquez-Pertejo, 2022d; CDC, 2019b; FDA, 2012).
Listeria Monocytogenes
Listeriosis is a foodborne disease that affects a small number of people compared to other organisms; however, it is a leading cause of death from foodborne disease. While most healthy people experience only mild gastroenteritis, the more severe invasive form results in an overall fatality rate of 15% to 30%. Among people with septicemia, the fatality rate is 50%; when meningitis occurs, the fatality rate is approximately 70%. Perinatal/neonatal infections have a fatality rate of 80%. Onset is rapid for the gastrointestinal form and occurs a few hours to 3 days after food ingestion. The invasive form, which results in septicemia and meningitis, has a variable incubation from 3 days to 3 months. Most patients' health status at onset is a predictor of disease severity. Healthy individuals are most likely to experience the gastroenteric form with a shorter duration. At the same time, people with chronic health problems, immunocompromise, or advanced age are prone to the invasive type (FDA, 2012).
The most common food sources are unpasteurized dairy products, soft cheeses, blue-veined cheese, deli meats, hot dogs, meat salads, unwashed raw vegetables, and refrigerated smoked seafood. Treatment consists of intravenous ampicillin (Omnipen) for at least 14 days. For those allergic to ampicillin (Omnipen), trimethoprim with sulfamethoxazole (Bactrim) is generally accepted. Listeria is salt-tolerant and can grow in temperatures below 34°F. It lives in moist environments, soil, and decaying vegetation throughout the natural environment. Listeria is highly tenacious. For example, in a single meat processing plant, the same strain was found first in 1989 and then 11 years later. Efforts to limit disease have led to declines over the last 20 years. Since Listeria contamination can include food workers, incoming air, raw materials, and food processing environments, all food production employees need sufficient education on effective control and prevention measures. In processing areas, the most significant risk involves cross-contamination after food is processed (FDA, 2012: Pfaff & Tillett, 2016).
Listeriosis presents a specific risk during pregnancy. Approximately 14% of cases affect pregnant women, who have a 10-fold risk compared to the general public. Immunologic changes during pregnancy increase susceptibility; the highest risk is during the third trimester. The bacteria target placental cell receptors. Transmission during pregnancy can happen directly from a pregnant patient or can be introduced to neonates as a nosocomial infection due to inadequate staff handwashing and surface hygiene. While its occurrence is rare, the consequences are extreme. Pregnant patients may not readily report symptoms, attributing them to flu-like illness, including headaches, gastritis, diarrhea, and backache; some experience severe abdominal pain and fevers. Sometimes, 2 months or more pass after infection before symptoms appear. As a precaution, any fever at or above 100.6°F in a pregnant patient with signs and symptoms of Listeria indicates the need for blood cultures. Even if the patient experiences mild to moderate symptoms, their fetus is greatly affected (e.g., via miscarriage, intrauterine fetal demise, neonatal meningitis, and death). Early onset symptoms for neonates include respiratory distress, poor muscle tone, pallor, meconium staining, and a diffuse, grainy rash that can develop into abscesses (granulomatosis infantiesepticum). Late-onset symptoms, with an average time of onset at 14 days after birth, generally involve the central nervous system and include irritability, lethargy, a stiff neck, fevers, and seizures (Pfaff & Tillett, 2016).
Additional Reportable Foodborne Diseases
Shigella
There are four genera of Shigella that cause inflammatory dysentery: A (S. dysenteriae), B (S. flexneri), C (S. boydii), and D (S. sonnei). S. sonnei is most common in the US. The only host is humans. Shigellosis is the sixth most common domestically acquired foodborne illness in the US, with 31% of cases foodborne. Contamination of food or water with human feces is the primary source. Raw foods, dairy products, poultry, and salads (e.g., tuna, potato, and macaroni) can transmit the disease. Food or fomites can spread bacteria indirectly, and flies can serve as vectors. The organism is sensitive and will break down quickly, so samples must be tested as quickly as possible for accuracy. Shigellosis (bacillary dysentery) is a common name for this illness. Diarrhea can consist of watery stool or, in severe cases, contain blood and mucus. Young children, the elderly, and immunocompromised people are more severely affected. In unsanitary conditions, the disease spreads rapidly. The onset of symptoms occurs 8 to 50 hours after ingesting contaminated food. Adults often experience abdominal pain, the urgency to defecate (tenesmus), and the passage of formed feces that temporarily relieves the pain. The severity of diarrhea is progressive, and the stools become liquid with mucus, pus, and sometimes blood. Severe tenesmus may result in rectal prolapse or consequent fecal incontinence. The disease is self-limiting, with mild disease resolving in 4 to 8 days, but more severe cases can take 3 to 6 weeks to resolve. Some patients have a sudden onset with liquid stools, vomiting, and severe dehydration or no symptoms before the onset of delirium, seizures, and coma. Their stool may be white liquid without fecal material, often described as rice-water stools; death may occur in 12 to 24 hours. Children have more severe symptoms and can die in the first 12 days if untreated. Initially, an infected child will have a fever, irritability, drowsiness, anorexia, nausea, vomiting, diarrhea, abdominal pain and distention, and tenesmus. Progression in 3 days changes to stool containing blood, pus, and mucus and may involve more than 20 stools per day with resulting weight loss and severe dehydration (Bush & Vasquez-Pertejo, 2022f; FDA, 2012).
Diagnostic testing consists of stool cultures, the presence of fecal leukocytes, an elevated WBC count (usually around 13,000), hemoconcentration, and indications of metabolic acidosis. Supportive care with fluid replacement is essential. For severely ill patients, antibiotics can be used. These may include a fluoroquinolone (e.g., ciprofloxacin [Cipro]), azithromycin [Zithromax]), or a third-generation cephalosporin (e.g., ceftriaxone [Rocephin]). Never give antidiarrheal drugs such as loperamide (Imodium), as these may prolong the illness. Meticulous handwashing by patients and caregivers is crucial. Clothes and bed linen require detergent and hot water for cleaning (Bush & Vasquez-Pertejo, 2022f).
Vibrio
Vibrio is a bacterium found in saltwater and brackish (mixed salt and fresh) waters. Raw or undercooked seafood, especially oysters, are the primary food source. The US has about 80,000 cases per year, with 500 hospitalizations and 100 deaths. Transmission occurs most often from May through October. Factors that increase the risk of Vibrio include immunosuppression, liver disease, cancer, diabetes, HIV, thalassemia, bariatric surgery (or any partial gastrectomy), and using medications to lower stomach acid. Vibrio organisms are susceptible to acidity, freezing, and cooking and are killed by common disinfectants, including bleach and alcohol (CDC, 2020b; FDA, 2012).
Cholera—the most severe foodborne disease caused by these bacteria—is caused by Vibrio cholerae. Contaminated water and seafood can cause acute small bowel infections. The bacteria produce an enterotoxin that causes the small bowel mucosa to hypersecrete an isotonic electrolyte solution. Patients often experience an abrupt onset of painless, rice-water diarrhea that can sometimes exceed one liter per hour. Vomiting is typical, but nausea is not. Hypovolemia, hypokalemia, and hemoconcentration occur, but serum sodium remains normal. Symptoms include extreme thirst, scant urine, muscle cramps, weakness, sunken eyes, and skin wrinkling on the fingers. Renal tubular necrosis, circulatory collapse with cyanosis, and stupor can occur without fluid replacement. Incubation is 1 to 3 days. While cases are rare, some people become chronic biliary tract carriers. Culture and serotyping of the stool are used for diagnosis. Rapid dipstick testing for cholera is available for public health purposes if laboratory testing is limited (CDC, 2020b; FDA, 2012).
Milder cases can be managed with standard rehydration, but severe cases require intravenous administration of isotonic fluids and potassium replacement to resolve hypokalemia, which is critical in pediatric clients. Once a patient is rehydrated, the fluid administration rate is based on stool volume. Oral rehydration solution (ORS) packets are available in areas where cholera is endemic. The packets contain 13.6 g glucose, 2.6 g sodium chloride, 2.9 g trisodium citrate dihydrate (or 2.5 g potassium bicarbonate), and 1.5 g potassium chloride, added to one liter of clean water. When packets are unavailable, six small spoons of sugar and one-half spoonful of salt can be substituted. The cessation of vomiting and return of appetite are indications that solid food can be resumed (Bush & Vasquez-Pertejo, 2022b; CDC, 2020b).
Vibrio vulnificus is much less common, with approximately 96 cases per year acquired in the US; it has a mortality rate of 35% in septicemia cases. The onset of V. vulnificus is 12 hours to 21 days, with a mean time to septicemia of 4 days. The mean duration of septic illness is 1.6 days, reflecting, to some extent, the high mortality rate once septicemia occurs. For healthy people, acute enteritis is usually mild and self-limiting, but susceptible people are at increased risk for septicemia. While other seafood and cross-contamination are risks, 90% of cases in the US are from eating raw Gulf Coast oysters. Factors that increase risk are chronic liver disease (including transplantation or liver cancer), medications and diseases causing immunosuppression, insufficient gastric acid, diabetes, renal disease, or intestinal disease. HCPs must teach people at risk to eat cooked seafood and take measures to decrease cross-contamination (CDC, 2019b; FDA, 2012).
The Vibrio species that cause less severe foodborne diseases include V. parahaemolyticus, V. mimicus, and V. hollisae, which are typically associated with inadequately cooked seafood, especially shellfish. V. parahaemolyticus is rarely transmitted by the fecal-oral route because the organism is damaged by freshwater. Symptoms typically include watery large-volume diarrhea, abdominal pain, weakness, and tenesmus. Less frequently, patients may exhibit nausea, vomiting, low-grade fevers, and bloody stools (which can contain granular leukocytes). The culture media used specifically for Vibrio is thiosulfate-citrate-bile salts-sucrose medium, and both the stool and the suspected food can be cultured. Treatment includes the replacement of a large amount of fluid and electrolytes lost. Antibiotics are not generally used, but for severe cases, ciprofloxacin (Cipro) or doxycycline (Vibramycin) can be given as a single dose. Oral cholera vaccines, such as Vaxchora, are available and recommended for people who plan to travel to endemic areas (Bush & Vasquez-Pertejo, 2022b, 2022e; FDA, 2012).
Clostridium Botulinum
Foodborne Clostridium botulinum has a hospitalization rate of approximately 83% and a fatality rate of 17%. Even with treatment, mortality is between 5% and 10%. The bacteria are anaerobic and produce a potent neurotoxin. The neurotoxin blocks motor nerve terminals at the neuromuscular junction, resulting in flaccid paralysis. Improperly home-canned foods are the most common source; it is more common in low-acid foods such as corn, peppers, green beans, beets, asparagus, and mushrooms. Other at-risk foods are tuna fish, chicken and chicken livers, liver pate, luncheon meats, lobster, and smoked or salted fish. The onset of the disease varies from 4 hours to 8 days but is typically between 18 and 36 hours. Neurologic symptoms begin early with diplopia, drooping eyelids, slurred speech, difficulty swallowing, a dry mouth, and muscle weakness. Neurologic progression is symmetrical and downward, starting at the head with eventual paralysis of the arms, trunk, legs, and respiratory muscles. Death from asphyxia can occur without immediate intervention when the diaphragm and chest muscles become involved. Early administration of botulinum antitoxin, available from the CDC, can improve outcomes. Mechanical ventilation may be necessary for weeks to months. While the symptoms are highly diagnostic, differentiation from other disorders may be difficult. Stool and serum can be tested for the toxin, but the most specific test is mouse neutralization, which takes 48 hours (CDC, 2019b; FDA, 2012).
The first sign of infant botulism is constipation. Subsequently, an affected infant exhibits a flat facial expression, poor feeding with weak sucking, a weak cry, decreased movement, difficulty swallowing, excessive drooling, progressive muscle weakness, and breathing problems. An antitoxin specific to infant botulism (BIG-IV) is available and should be administered early. Supportive treatment is given with the implementation of mechanical ventilation and intensive care for weeks to months. While many items may be risks, honey is one food specifically linked to incidence. HCPs should teach parents and caregivers about not giving honey to any child under 12 months of age. An adult form of botulism similar to infant botulism can affect patients with a surgical alteration of the gastrointestinal system or on antibiotic therapy (FDA, 2012).
Brucella
As a foodborne disease, brucellosis in the US is most frequently contracted from consuming imported raw milk or soft cheese products made from raw goat or cow milk. Humans are more likely to contract the species Brucella meletensis, which is from goats. The disease burden is the greatest in endemic countries where goats are raised, and there is no pasteurization. A zoonotic transfer (infectious disease spread from an animal species to a human) occurs, with raw milk being the most common source. However, another source is human contact with the reproductive parts of infected animals. Human-to-human transfer is rare but has occurred through reproduction and breastfeeding. Among animals, spontaneous abortion is a common symptom; for humans, this is rare. Pasteurization of milk (mandated by law since 1947), along with surveillance and control measures, has minimized the risk of this disease from food products in the US. The onset of symptoms is generally within 3 weeks but can be longer (FDA, 2012).
Brucellosis was once known as undulant fever because of intermittent fevers and sweating. Septicemia happens at the beginning of the illness. Without treatment, the disease can become chronic with the recurrence of febrile illness. The development of brucellar spondylitis, a focalization of brucellosis in the bones (especially in the lumbar vertebrae), can also occur. Diagnostic tests include isolating the organism from blood or bone marrow, testing for anti-Brucella antibodies, and radiologic examination for vertebral changes and bone spurs. An aggressive combination antibiotic treatment for up to 6 weeks can prevent relapses in up to 90% of patients. The most common combinations are doxycycline (Vibramycin) plus rifampin (Rifadin) or doxycycline (Vibramycin) plus streptomycin (Streptomycin; FDA, 2012).
Francisella Tularensis
Two types of F. tularensis, type A and B, cause tularemia. Type A is found primarily in rabbits and rodents, is more virulent, and occurs mainly in the US and Canada. Food can be contaminated; however, other routes include bites of arthropod vectors (e.g., deer flies, ticks, and fleas), inhalation, and direct contact with infected tissues or material. Animal meat, especially undercooked meat from rabbits and hares, and milk can be food sources. The other risk involves rodent droppings contaminating the food. It is among the most infectious microorganisms because inhaling as few as 10 bacteria cells can lead to infection with a high mortality rate; in foodborne cases, over 1 million are required. The onset of symptoms can be from 1 day to a week but is typically 3 to 6 days. Some of the organisms are more virulent, and this factor influences outcomes. Infected food can cause either oropharyngeal infection, which causes pharyngitis and necrotic cervical adenopathy, or gastrointestinal infection, with a range of symptoms from mild diarrhea to severe bowel damage. Diagnosis includes confirmation made by culture on enriched media, but real-time PCR, direct fluorescent antibody (DFA), and ELISA-based techniques are used for preliminary diagnosis. Leukocytosis or only an elevation in the proportion of neutrophils, eosinophils, and basophils in the CBC provides evidence of infection. Streptomycin (Streptomycin) injectable is used for tularemia in severe cases. Foodborne tularemia is rare in the US. Any form can spread to the lungs or meninges, causing severe disease and increased mortality (Bush & Vasquez-Pertejo, 2022g; FDA, 2012).
Hepatitis A
Hepatitis A (HAV) has an estimated hospitalization rate of 37.5% and a death rate of 2.4%. With the implementation of the hepatitis vaccine, there was a 95% decrease in incidence from 1995 to 2011. However, from 2015 to 2019, the incidence increased by 1,325%; the increase in 2019 was due to unprecedented person-to-person outbreaks reported in 31 states among people who use intravenous drugs and those experiencing homelessness. In addition, the CDC identifies other people at risk for HAV: travelers to countries with high or endemic HAV, men who have sex with men, people with clotting factor disorders, people who work with primates, and people with adopted children from countries with high or intermediate endemic HAV. Hepatitis A is a hardy virus that can survive freezing; food must be cooked to above 185°F for at least 1 minute. The virus can live for months in environments with poor sanitation and improper sewage disposal (CDC, 2019b, 2020c, 2021; Walker, 2018).
People with HAV may be asymptomatic (especially children under 6), or it can be a severely disabling disease. Incubation is typically 28 days but can range from 15 to 50 days. In adults, the onset is usually abrupt with abdominal pain, a fever, malaise, anorexia, nausea with or without vomiting, and diarrhea. The progression of the disease is characterized by liver symptoms that include jaundice, dark urine, clay-colored stool, and hepatomegaly. Diagnosis consists of a blood test for serum immunoglobulin M (IgM) anti-HAV antibodies that are detectable 5 to 10 days after exposure. Reverse transcriptase-polymerase chain reaction (RT-PCR) may also be used to detect HAV ribonucleic acid (RNA). Fulminate hepatitis can occur with liver failure, particularly in patients with chronic liver disease. Mortality in these cases is 70% to 80%. Throughout the disease course, a patient's liver status can be established by tests for serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and bilirubin. Physical care during the disease includes adequate rest, a diet of small meals that are high-calorie and high-protein (based on liver status), and modification of medications metabolized by the liver as directed by the HCP. Environmental care includes routine handwashing with soap and water for 15 to 20 seconds, no sharing of eating utensils or toothbrushes with family members, wearing gloves, and disinfecting bed linens, bathroom surfaces, and laundry used by the patient. After recovery, serum IgG antibodies are present, and immunity is lifelong (CDC, 2021; FDA, 2012; Walker, 2018).
Vaccination has made HAV a preventable disease. Children aged 12 to 18 months should receive two doses of Havrix or Vaqta, with the second dose 6 to 18 months after the initial dose. These vaccines can also be given to adults exposed to HAV. For general prevention among adults, three doses of the Twinrix vaccine that includes both hepatitis A and hepatitis B are given; the second dose is given 1 month after the initial dose, and the third dose is given 6 months later. If a person has travel planned with risk for exposure, four doses of Twinrix can be given with three doses in 21 days (initial, day 7, and day 21 to 30) and the fourth dose at 12 months after the initial dose. Hepatitis A vaccine can be given during pregnancy. Neither healthcare workers nor food service workers need routine vaccination against HAV. Immune globulin can be administered to people exposed to HAV but must be administered within 2 weeks of exposure (CDC, 2021).
Cryptosporidium
Based on serologic surveys, an estimated 80% of the US population has had cryptosporidiosis. The organism, an oocyte, is half the size of a red blood cell and requires as few as 10 to cause an infection. Ingested food and water are likely sources. Still, pool water is a major vehicle, as the organism is extremely tolerant of chlorine and can exist for long periods in the presence of bleach. Infection from person to person by the fecal-oral route is common. Fresh produce is the most common food source, but juices and milk may also be infected. Once in the body, Cryptosporidium differentiates into two forms; thick-walled organisms are shed in the stool, and thin-walled organisms break down in the intestinal wall and can cause symptoms (FDA, 2012).
The onset of symptoms is typically 1 week, and 80% of those infected have symptoms. The onset is usually sudden for immunocompetent people, with profuse, watery diarrhea and abdominal cramping. Occasionally, the person may have nausea, anorexia, a fever, and malaise. Symptoms typically resolve in 1 to 2 weeks but may last for a month. Caution should be advised because the organism is shed in stools for several weeks after symptoms have resolved. Symptom onset for immunocompromised patients is much more gradual, but the diarrhea is more severe, with fluid losses of more than 5 to 10 liters per day for AIDS patients. Diarrhea can become intractable and may persist for life for these patients. A CD4 count of fewer than 180 cells/mm3 is the trigger point for the greatest risk for severe and protracted disease in AIDS patients. Diagnostic testing includes microscopic stool examination of multiple samples using phase-contrast microscopy, staining with modified Ziehl-Neelsen or Kinyoun techniques, as well as immunofluorescence microscopy with fluorescein-labeled monoclonal antibodies. Specific enzyme immunoassay for fecal Cryptosporidium provides greater sensitivity than microscopic examination alone. Intestinal biopsies can reveal Cryptosporidium in digestive epithelial cells (FDA, 2012; Marie & Petri, 2022a).
Cyclospora Cayetanensis
Cyclospora cayetanensis is a protozoan parasite shed in vertebrates' feces. It requires 1 to 2 weeks outside the body (i.e., in the environment) to mature and become infective. The disease is more common in tropical and semi-tropical climates, especially during the rainy season. Outbreaks in the US have been associated with contaminated fresh vegetables, including prewashed salad mixes, basil, snow peas, and cilantro. Symptom onset happens 7 to 10 days after ingestion. The diarrhea is watery, can be explosive, and is accompanied by abdominal pain and bloating. While some patients are asymptomatic, others have severe, flu-like symptoms with headaches, vomiting, fevers, and general aching. AIDS patients are at risk for developing severe, intractable, voluminous diarrhea, as well as extraintestinal disease that includes cholecystitis and disseminated infection. Diagnosis includes identifying the organism in stool using Ziehl-Neelsen or Kinyoun acid-fast staining technique, as a unique quality of the organism is auto-fluorescence. More than three stool specimens may be necessary because cyst secretion is intermittent. A biopsy of intestinal tissue can reveal intracellular parasite stages. Treatment is with trimethoprim/sulfamethoxazole (Bactrim), and AIDS patients require higher doses and a longer duration of treatment. Death is extremely rare, but symptoms can last for months without treatment, and relapses are possible (FDA, 2012; Marie & Petri, 2022b).
Trichinella
Trichinosis is a parasitic infection in which at least a male parasite and a female parasite are ingested via infected meat. These parasites spend a day or two in the epithelium of the small intestine. Within 3 days, the newborn larvae they produced are shed into the intestine. From there, the larvae migrate to the liver, lung, eye, heart, and brain but can only survive long-term in skeletal muscle. Once in skeletal muscle, the larvae live until the animal dies or is eaten. Any animal that eats meat can be at risk, but the most common food source for humans has been pork. In the US, changes in pork production have contributed to the decreased incidence of trichinosis; this includes a requirement to cook any meat product fed to pigs, prevention of rodent contamination in pig enclosures, and required surveillance for Trichinella. Even with these measures, raw pork should always be cooked thoroughly (to an internal temperature greater than 160°F). Commercial freezing to a lower temperature can also destroy the larvae, but home freezing is insufficient and should never be considered effective for eliminating Trichinella from wild animal meat. Cases in the US have included walrus, bear, cougar, and other wildlife meats (FDA, 2012).
Symptoms of nausea, abdominal cramping, and diarrhea begin when newborn larvae increase in number in the digestive system. As the larvae migrate, systemic symptoms occur, including periorbital edema, myalgia, a persistent fever (greater than 102 °F), headaches, petechiae, and subconjunctival hemorrhages. Eye pain and photophobia frequently occur before chronic myalgia. An increase in eosinophil count begins when the larvae invade tissues, peaks 2 to 4 weeks after infections, and decreases once the larvae become encysted in the muscle cells. The larvae that do not reach muscle tissue eventually die, but large numbers present and dying in tissue can result in cardiac, neurologic, or pulmonary complications with possible death. Enzyme immunoassay is the fastest test to confirm the diagnosis. Laboratory measurement of increased creatine kinase and lactic dehydrogenase is found in 50% of patients. Muscle biopsy is usually not necessary but can be performed for species identification. Early treatment with an anthelmintic, such as albendazole (Albenza) or mebendazole (Vermox), can eliminate adult worms. Once the larvae reach muscle tissue, the medication may not kill the larvae, and larger doses have adverse effects. Analgesics to relieve muscle pain may be given. Some patients experience an allergic response to the larvae; when the myocardium or the central nervous system is involved, prednisone (Deltasone) may be given (Pearson, 2020b).
Common Foodborne Diseases That Do Not Require Reporting
Yersinia
Yersinia has a hospitalization rate of 34%, with an estimated death rate of 2%. The two most common species of Yersinia that cause gastroenteritis are Y. enterocolitica and Y. pseudotuberculosis. It is transmitted by the fecal-oral route, and the organism is found in animals (pigs, birds, beavers, cats, and dogs) and insects (fleas, flies, and frogs). Refrigeration does not kill the organism. Foods that primarily carry Yersinia are meats (especially pork), seafood, and unpasteurized milk. The spread of the organism can occur when handling meat products, during storage, or with poor sanitation and improper sterilization. In the home, handwashing and exclusive use of a cutting board for meat with a separate board for other products can decrease risk. Foods like chitlins that are prepared at home and include pork intestines are a known risk. Persons preparing these foods should avoid all physical contact with young children. For adult patients, the disease consists of self-limiting diarrhea. Children under 5 years old exhibit fevers, abdominal pain, diarrhea, and vomiting. Some children complain of headaches and a sore throat at the onset of the disease, and some may experience bloody stools. Abdominal pain frequently affects the right lower quadrant, and differentiation from appendicitis can be challenging, but yersiniosis has a much higher rate of diarrhea. Unnecessary appendectomies have been performed without adequate diagnostic consideration of yersiniosis (CDC, 2019b, 2019d; FDA, 2012).
Specimens of feces, blood, or vomit can be tested for Yersinia in patients with symptoms that indicate possible infection. Serology for biotype and PCR methods of molecular-based assays can be used to confirm. Treatment for gastroenteritis is supportive. Complications tend to affect people with the human immunologic leukocyte antigen, HLA-B27. These include reactive arthritis, glomerulonephritis, endocarditis, erythema nodosum, uveitis, and thyroid disorders. Reactive arthritis can occur in asymptomatic patients. Bacteremia is a rare complication. Antibiotics such as gentamicin (Garamycin) or cefotaxime (Claforan) may be given for septicemia or other complications (CDC, 2019c; FDA, 2012).
Bacillus Cereus
Foodborne Bacillus cereus affects approximately 63,000 people annually in the US. It has two types based on the predominant symptom: diarrheal and emetic. The diarrheal form has an incubation of 6 to 15 hours, followed by watery diarrhea, abdominal cramps, and occasionally nausea. The emetic form has an incubation of 30 minutes to 6 hours, followed by nausea and vomiting. Both forms are usually self-limited and resolve within 24 hours. A cytotoxin was found in a strain of B. cereus that caused a severe outbreak and three deaths. Local and systemic infections of B. cereus can provoke pyogenic infections, gangrene, sepsis, meningitis, cellulitis, panophthalmitis, lung abscesses, infant death, and endocarditis. Outbreaks have been attributed to various foods, including rice, beef, turkey, beans, and vegetables; food mixtures such as sauces, casseroles, and soups have also been implicated. Diagnosis is based on the isolation of the organism from food or patient feces or vomit. The emetic enterotoxin of B. cereus has been implicated in the development of liver failure in otherwise-healthy individuals (CDC, 2019b; FDA, 2022c; Foodsafety.gov, 2021).
Viral Conditions
Astrovirus, rotavirus, sapovirus (SaV), and hepatitis E are viral gastrointestinal illnesses that do not require reporting to the CDC or state agencies. They are all transmitted by the fecal-oral route, and most are spread from person to person, with food handlers at the greatest risk for spreading. Fecal contamination of water where food is obtained is also a source. In 2012 and 2014, the largest outbreak in Europe occurred, with 1,500 patients in 13 European countries due to frozen berries. Foodborne transmission of the hepatitis E virus is increasing, with processed pork, wildlife meat, and shellfish as the major sources. SaV is similar to NoV; it is found in shellfish but rarely transmitted through food. SaV does not bind to HGBAs, and no susceptibility pattern occurs with NoV. Rotavirus and astrovirus are also rarely foodborne but are transmitted person-to-person. Emerging viruses with the potential for foodborne transmission include SARS coronavirus, H1N1 influenza, and Zika virus. While food consumption is a risk, people who handle food also risk cutaneous transmission. Although fecal matter is the primary source, nurses must understand that viruses can also be spread through urine, saliva, and breast milk (CDC, 2019b).
Before vaccination, rotavirus was the most common viral foodborne infection in young children. In 95 countries, a 49% to 89% decrease in hospital admission for rotavirus and an overall 17% to 55% decrease in all hospital admissions for gastroenteritis in children under age 5 occurred within 2 years of the immunization being initiated. Without immunization, children are at greatest risk from ages 4 to 23 months. Food contaminated with feces from an infected person is the transmitting agent. Diarrhea and vomiting are typical; without rehydration, this can progress to hypovolemic shock, coma, and death. Unlike NoV, rotavirus immunity progresses with each subsequent infection. The rotavirus vaccine decreases incidence by limiting both infections and the shedding of the organism. Diagnosis of even subclinical cases is possible with the detection of viral nucleic acid (CDC, 2019b).
In developed countries, rotavirus is more common in winter, but undeveloped countries have no seasonality. A lack of adequate rehydration therapies results in severe illness, and 90% of the 200,000 deaths worldwide happen in developing countries. Treatment with antimotility drugs is not recommended. Probiotics with Lactobacillus rhamnosus strain GG, Lactobacillus reuteri, and Saccharomyces boulardi can decrease the duration of diarrhea. Continuation of breastfeeding or resumption of feeding after rehydration is recommended for children younger than 6 months. Zinc supplementation is an added recommendation in developing countries. Both of the rotavirus vaccines for use in infants are oral drops. RotaTeq (RV5) is given in three doses at 2 months, 4 months, and 6 months. Rotarix (RV1) is given in two doses at 2 months and 4 months. The vaccine should not be given after 8 months, even if dosing is incomplete. Contraindications include an allergic response to the vaccine, immunodeficiency, or a history of intussusception. A vaccine dose should be postponed if a child has moderate or severe illness, including diarrhea or vomiting. Side effects of the vaccine include irritability, mild diarrhea, or vomiting. Adverse effects include a risk for intussusception, which usually occurs within a week after the first or second dose (Banyai et al., 2018; Savoy, 2022).
Non-infectious Foodborne Diseases
Food is a daily requirement of all humans. The following examples are a reminder that risks can be present beyond infectious disease.
Mercury Poisoning
Most HCPs know the risk of mercury poisoning from fish during pregnancy. While mercury exposure should be minimized for everyone, it is most critical during pregnancy because it is linked to changes in fetal brain development. Microorganisms in water process inorganic and elemental mercury and deposit an organic compound—methylmercury—in the tissue of fish. Fish that eat other fish and have a longer lifespan accumulate more mercury and are at the greatest risk. Fish in this category include orange roughy, king mackerel, marlin, shark, swordfish, tilefish, and bigeye tuna. These should be avoided, especially during pregnancy. During fetal development, exposure to methylmercury is known to result in abnormalities and cerebral palsy. Chronic exposure at other ages results in neurologic damage. Current recommendations for nutrition during pregnancy include a maximum of 8 to 12 ounces of low-mercury fish per week, such as catfish, cod, flounder, salmon, sardines, shrimp, light tuna, tilapia, and trout (CDC, 2017; FDA, 2020, 2022a).
Arsenic Poisoning
Rice is a major food source worldwide. Inorganic arsenic occurs in rice, even in countries like the US, where water has a low arsenic content. Inorganic arsenic is carcinogenic to the bladder, lungs, skin, and prostate. Signes-Pastor and colleagues (2019) found an elevated risk of arsenic poisoning with the intake of brown rice, which is associated with a risk of bladder cancer. Arsenic also increases the risk of developing heart disease. Immediate arsenic poisoning symptoms include muscle cramping, gastrointestinal problems, and hands and feet lesions. Current experimentation to decrease this risk focuses on identifying and growing rice varieties that absorb less arsenic from the soil and water. The recommended safe intake for adults is no more than two or three servings of rice each week. Traditionally, rice has been cooked with equal parts of water and rice; cooking rice with three times as much water as rice and rinsing the rice before and after cooking can decrease the arsenic content by 30% (Signes-Pastor et al., 2019).
Scombroid Syndrome
Scombroid syndrome occurs when histamines contaminate fish. Approximately 5% of food poisoning cases in the US are from scombroid syndrome. Bacteria in fish gills and gastrointestinal tracts impart histamine. Scombridae and Scomberesocidae families of fish are the usual source; this group includes tuna, mackerel, albacore, sardines, anchovies, and mahi-mahi. Neither food processing nor cooking eliminates histamine from fish. The onset of symptoms is approximately 10 to 30 minutes after ingestion and usually resolves in 24 hours. Infection is self-limiting but can last several days. Flushing, sometimes accompanied by hives and edema, can be confused with a fish allergy. Scombroid syndrome symptoms include abdominal pain, diarrhea, nausea, vomiting, headaches, dizziness, and palpitations. Some people experience a metallic, peppery, or bitter taste sensation; rarely, wheezing and hypotension occur. Diagnosis includes history taking and histamine testing of the patient's plasma and from the fish. Patients on isoniazid and monoamine oxidase inhibitors are at increased risk of scombroid syndrome. Administration of rapid-acting antihistamines targets the cause, and symptomatic treatment (i.e., intravenous fluids and H1 or H2 antihistamines for gastrointestinal irritation and nausea) can be used (FDA, 2017; Ridolo et al., 2016).
Foodborne Disease Control Measures in the Home
The home is both a setting for food preparation and a shared environment for people with various risks and exposures. While this is evident globally, food safety and handling in the US have experienced changes that lead to increased risk. The FDA (2018a) compiles current data and research on foodborne disease trends in the US. Lando and colleagues (2018) researched the utilization of cell phones during food preparation. Mobile devices are used constantly, and there was decreased likelihood of handwashing before and after touching the device, which increases the risk of contamination with foodborne organisms. The aging of the population and the increase in people with immunocompromise living at home have increased the risk of foodborne disease. Two groups have shown the best food handling practices at home: those born before 1940, when foodborne disease was more prevalent, and those who were young adults during the E. coli OH157:H7 outbreak in the early 1990s. The availability of products such as donor breast milk necessitates education to ensure that risks for disease transmission are minimized by pasteurization, screening of donors, and correct handling in the home (Moreno, 2016). Current public health education exemplifies the need for changing habits to improve food safety, including avoiding eating anything containing raw flour, such as dough; raw flour may be contaminated with organisms and has not been treated to inhibit disease. The CDC and FDA provide information on food safety for home use. Figure 2 and Figure 3 are examples of teaching tools that target the risk of foodborne illness by encouraging safer food handling practices (CDC, 2018b, 2022c; FDA, 2022b).
Figure 2
Food Safe Shopping and Storage

(FDA, 2018c)
Figure 3
Food Safe Meal Prep
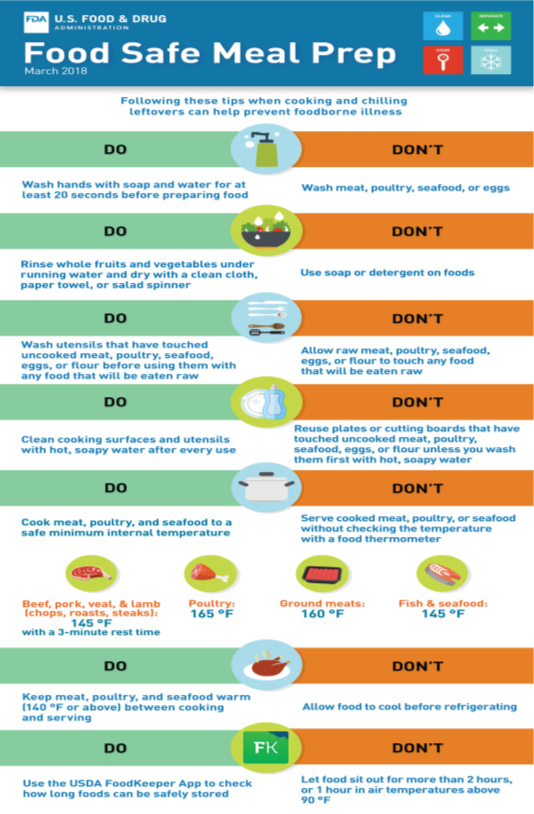
(FDA, 2018b)
Evans and Redmond (2018) evaluated oncology patients' knowledge and food-handling practices at home. Patients with cancer are more at risk for severe consequences of foodborne organisms, with 15% to 25% of serious Salmonella infections occurring in this population. Recommendations that are good practice with the general population but essential for oncology patients include strict adherence to use-by dates on ready-to-eat food, eating ready-to-eat food within 2 days of opening, ensuring temperatures of refrigerators are at or below 41°F (using a thermometer for accuracy), and avoiding raw or undercooked foods, especially seafood, eggs, meat, soft cheeses, and unpasteurized dairy products. A thermometer is also necessary to ensure meat and other foods reach an internal temperature of 145°F to 165°F. Reviews of handwashing need to include using hot water and soap; rubbing all hand surfaces, including the palms, back of hand, and fingers; and drying hands only on paper towels. Household cleaning practices and areas of highest risk should be reviewed. Family members and patients should be taught food safety practices to implement before and during chemotherapy treatment (Evans & Redmond, 2018).
One of the new areas of concern for introducing foodborne illness in the home is the use of probiotics and prebiotics. These products are considered food or dietary supplements in the US and are generally regarded as safe (GRAS). Products with this status per the FDA are not subjected to close monitoring. A lack of standardization of the number and type of cultures used and minimal quality control increases potential effects, especially among pediatric patients where use is increasing. Specific risks involve contamination, with a case study involving a premature infant's death from a fatal gastrointestinal mucormycosis related to a contaminated commercial dietary supplement. Other general risks include systemic infections, the production of toxins by the probiotic organisms, gene transfer of antibiotic resistance, and unpredicted changes in the immune system. Recommendations to improve quality control for all probiotics and establish standards for probiotic preparation for clinical indications have been proposed to decrease these risks (Kolacek et al., 2017).
References
Banyai, K., Estes, M., Martella, V., & Parashar, U. D. (2018). Viral gastroenteritis. The Lancet, 392, 175–186. https://doi.org/10.1016/S0140-6736(18)31128-0
Bush, L. M., & Vazquez-Pertejo, M. T. (2021a). Clostridium perfringens food poisoning. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/anaerobic-bacteria/clostridium-perfringens-food-poisoning
Bush, L. M., & Vazquez-Pertejo, M. T. (2021b). Overview of clostridial infections. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/anaerobic-bacteria/overview-of-clostridial-infections
Bush, L. M., & Vazquez-Pertejo, M. T. (2021c). Staphylococcal infections. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-positive-cocci/staphylococcal-infections#v26288251
Bush, L. M., & Vazquez-Pertejo, M. T. (2022a). Campylobacter and related infections. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/campylobacter-and-related-infections
Bush, L. M., & Vasquez-Pertejo, M. T. (2022b). Cholera. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/cholera
Bush, L. M., & Vasquez-Pertejo, M. T. (2022c). Escherichia coli infections. Merck Manual Professional Version. https:/www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/escherichia-coli-infections
Bush, L. M., & Vasquez-Pertejo, M. T. (2022d). Infection by Escherichia coli 0157:H7 and other enterohemorrhagic E. coli (EHEC). Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/infection-by-escherichia-coli-o157-h7-and-other-enterohemorrhagic-e-coli-ehec
Bush, L. M., & Vazquez-Pertejo, M. T. (2022e). Noncholera vibrio infections. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/noncholera-vibrio-infections
Bush, L. M., & Vasquez-Pertejo, M. T. (2022f). Shigellosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/shigellosis
Bush, L. M., & Vasquez-Pertejo, M. T. (2022g). Tularemia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/gram-negative-bacilli/tularemia
Centers for Disease Control and Prevention. (2017). Mercury fact sheet. National Biomonitoring Program. https://www.cdc.gov/biomonitoring/Mercury_FactSheet.html
Centers for Disease Control and Prevention. (2018a). Estimates of foodborne illness in the United States: Burden of foodborne illness: Findings. https://www.cdc.gov/foodborneburden/2011-foodborne-estimates.html
Centers for Disease Control and Prevention. (2018b). Food safety: Information for health departments. https://www.cdc.gov/foodsafety/groups/health-departments.html
Centers for Disease Control and Prevention. (2018c). Staphylococcal (staph) food poisoning. https://www.cdc.gov/foodsafety/diseases/staphylococcal.html
Centers for Disease Control and Prevention. (2018d). Steps in a foodborne outbreak investigation [Image]. https://www.cdc.gov/foodsafety/outbreaks/investigating-outbreaks/investigations/index.html
Centers for Disease Control and Prevention. (2019a). Food safety: People with a higher risk of food poisoning. https://www.cdc.gov/foodsafety/people-at-risk-food-poisoning.html
Centers for Disease Control and Prevention. (2019b). NCEZID: Foodborne disease (food poisoning). National Center for Emerging and Zoonotic Infectious Disease. https://www.cdc.gov/ncezid/what-we-do/our-topics/foodborne-disease.html
Centers for Disease Control and Prevention. (2019c). Yersinia enterocolitica (Yersiniosis): Information for health & lab professionals. https://www.cdc.gov/yersinia/faq.html
Centers for Disease Control and Prevention. (2019d). Yersinia enterocolitica (Yersiniosis): Questions and answers. https://www.cdc.gov/yersiia/faq.html
Centers for Disease Control and Prevention. (2020a). Food safety: Foodborne germs and illnesses. www.cdc.gov/foodsafety/foodborne-germs.html
Centers for Disease Control and Prevention. (2020b). Vibrio species causing vibriosis: Information for health professionals and laboratorians. https://www.cdc.gov/vibrio/healthcare.html
Centers for Disease Control and Prevention. (2020c). Viral hepatitis: Hepatitis A questions and answers for health professionals. https://www.cdc.gov/hepatitis/hav/havfaq.htm#general
Centers for Disease Control and Prevention. (2021). Viral hepatitis: Surveillance for viral hepatitis – United States, 2019. https://www.cdc.gov/hepatitis/statistics/2019surveillance/HepA.htm
Centers for Disease Control and Prevention. (2022a). Campylobacter (campylobacteriosis): Information for health professionals. https://www.cdc.gov/campylobacter/technical.html
Centers for Disease Control and Prevention. (2022b). Food safety: Food poisoning symptoms. www.cdc.gov/foodsafety/symptoms.html
Centers for Disease Control and Prevention. (2022c). Foodborne outbreaks: List of selected multistate foodborne outbreak investigations. https://www.cdc.gov/foodsafety/outbreaks/multistate-outbreaks/outbreaks-list.html
Centers for Disease Control and Prevention. (2022d). Salmonella: Information for healthcare professionals and laboratories. https://www.cdc.gov/salmonella/general/technical.html
Centers for Disease Control and Prevention. (2022e). Typhoid fever and paratyphoid fever: Symptoms and treatment. https://www.cdc.gov/typhoid-fever/symptoms.html
Evans, E. W., & Redmond, E. (2018). Food safety knowledge and self-reported food-handling practices in cancer treatment. Oncology Nursing Forum, 45(5), E98–E110. https://doi.org/10.1188/18.NOF.E98-E110
Facciola, A., Riso, R., Avventuroso, E., Visalli, G., Delia, S. A., & Lagana, P. (2017). Campylobacter: From microbiology to prevention. Journal of Preventive Medicine and Hygiene, 58(2), E79–E92. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5584092/
Foodsafety.gov. (2021). Bacillus cereus. US Department of Health and Human Services. https://foodsafety.gov/food-poisoning/bacteria-and-viruses#bacillus-cereus
Gotfried, J. (2021a). Overview of gastroenteritis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gastrointestinal-disorders/gastroenteritis/overview-of-gastroenteritis
Gotfried, J. (2021b). Traveler’s diarrhea. Merck Manual Professional Version. https://www.merckmanuals.com/professional/gastrointestinal-disorders/gastroenteritis/traveler’s-diarrhea
Heavey, E. (2018). Toxoplasmosis update. Nursing, 48(7), 62–64. https://doi.org/10.1097/01.NURSE.0000534106.04143.54
Hinkle, J. L., Cheever, K. H., Overbaugh, K. (2022). Textbook of medical-surgical nursing (15th ed.). Wolters Kluwer.
Kadariya, J., Smith, T., & Thapaliya, D. (2014). Staphylococcus aureus and staphylococcal foodborne disease: An ongoing challenge in public health. BioMed Research International, 2014(article 82965), 1-9. https://doi.org/10.1155/2014/827965
Kazanjian, P. (2018). The short-lived epidemic of botulism from commercially canned food in the United States, 1919–1925. Annals of Internal Medicine, 168(8), 579–584. https://doi.org/10.7326/M17-2853
Kolacek, S., Hojsak, I., Canani, R. B., Guarino, A., Indrio, F., Orel, R., Pot, B., Shamir, R., Szajewska, H., Vandenplas, Y., van Goudoever, J., Weizman, Z., & ESPGHAN Working Group for Probiotics and Prebiotics. (2017). Commercial probiotic products: A call for improved quality control. A position paper by the ESPGHAN working group for probiotics and prebiotics. Journal of Pediatric Gastroenterology and Nutrition, 65(1), 117–124. https://doi.org/10.1097/MPG.0000000000001603
Lando, A. M., Bazaco, M. C., & Chen, Y. (2018). Consumers’ use of personal electronic devices in the kitchen. Journal of Food Protection, 81(3), 437-443. https://doi.org/10.4315/0362-028X.JFP-17-172
Lee, F. (2017). Diagnostics and laboratory role in outbreaks. Current Opinion in Infectious Diseases, 30(4), 419–424. https://doi.org/0.1097/QCO.0000000000000388
Marie, C., & Petri, W. A., Jr. (2022a). Cryptosporidiosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/intestinal-protozoa-and-microsporidia/cryptosporidiosis?query=cryptosporidium
Marie, C., & Petri, W. A., Jr. (2022b). Cyclosporiasis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/intestinal-protozoa-and-microsporidia/cyclosporiasis?query=cyclosporiasis
Moreno, M. A. (2016). Donor breast milk. Journal of the American Medical Association, Pediatrics, 170(7), 720. https://doi.org/10.1001/jamapediatrics.2015.2540
National Institute of Diabetes and Digestive and Kidney Diseases. (2019). Definitions & facts of food poisoning. National Institutes of Health. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/definition-facts
O’Brien, S. J. (2017). The consequences of Campylobacter infection. Current Opinion in Gastroenterology, 33(1), 14–20. https://doi.org/10.1097/MOG.0000000000000329
Pearson, R. D. (2020a). Toxoplasmosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/extraintestinal-protozoa/toxoplasmosis
Pearson, R. D. (2020b). Trichinosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/nematodes-roundworms/trichinosis
Pfaff, N. F., & Tillet, J. (2016). Listeriosis and toxoplasmosis in pregnancy: Essentials for healthcare providers. Journal of Perinatal & Neonatal Nursing, 30(2), 137–138. https://doi.org/10.1097/JPN.0000000000000164
Qasmieh, S., Quinn, A., & Ries, A. (2018). Letters: Lessons learned about rapid diagnostic testing of stool. American Journal of Health-System Pharmacy, 75(21), 1690–1691. https://doi.org/10.2146/ajhp180514
Ridolo, E., Martignago, I., Senna, G., & Ricci, G. (2016). Scombroid syndrome: It seems to be fish allergy but… it isn’t. Current Opinions in Allergy and Clinical Immunology, 16(5), 516–521. https://doi.org/10.1097/ACI.0000000000000297
Robertson, P., Smith, A., Anderson, M., Stewart, J., Hamilton, K., McNamee, S., & Curran, E. T. (2017). American Journal of Infection Control, 45(2017), 440-442. https://doi.org/10.1016/j.ajic2016.11.024
Sabry, M., Abd El-Moein, K., Hamza, E., & Abdel Kader, F. (2016). Abstract: Occurrence of clostridium perfringens types A, E, and C in fresh fish and its public health significance. Journal of Food Protection, 79(6), 994–1000. https://doi.org/10.4315/0362-028X.JFP-15-569
Savoy, M. L. (2022). Rotavirus vaccine. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/immunization/rotavirus-vaccine
Signes-Pastor, A. J., Zens, M. S., Seigne, J., Schned, A., & Karagas, M. R. (2019). Rice consumption and incidence of bladder cancer in the United States population. Epidemiology, 30(2), e4–e5. https://doi.org/10.1097/EDE.0000000000000955
Suijkerbuijk, A. W. M., Bouwknegt, M., Mangen, M. J. J., de Wit, G. A., van Pelt, W., Bijkerk, P., & Friesema, I. H. M. (2016). The economic burden of a Salmonella Thompson outbreak caused by smoked salmon In the Netherlands. The European Journal of Public Health, 27(2), 325–330. https://doi.org/10.1093/eurpub/ckw205
US Food and Drug Administration. (2012). Bad bug book. https://www.fda.gov/food/foodborne-pathogens/bad-bug-book-second-edition
US Food and Drug Administration. (2017). Scombrotoxin poisoning and decomposition. https://www.fda.gov/food/seafood-guidance-documents-regulatory-information/scombrotoxin-poisoning-and-decomposition
US Food and Drug Administration. (2018a). Consumer research on foodborne illness. https://www.fda.gov/food/cfsan-consumer-behavior-research/consumer-research-foodborne-illness
US Food and Drug Administration. (2018b). Food safe meal prep [Image]. https://www.fda.gov/files/food/published/Food-Safe-Meal-Prep-Tips_Download.pdf
US Food and Drug Administration. (2018c). Food safe shopping & storage [Image]. https://www.fda.gov/files/food/published/Food-Safe-Shopping---Storage-Tips_Download.pdf
US Food and Drug Administration. (2020). People at risk of foodborne illness. https://www.fda.gov/food/consumers/people-risk-foodborne-illness
US Food and Drug Administration. (2022a). Advice about eating fish. https://www.fda.gov/media/73720/download
US Food and Drug Administration. (2022b). Food safety in your kitchen. https://www.fda.gov/food/buy-store-serve-safe-food/food-safety-your-kitchen
US Food and Drug Administration. (2022c). What you need to know about foodborne illnesses. https://www.fda.gov/food/consumers/what-you-need-know-about-foodborne-illnesses
Walker, B. W. (2018). Hepatitis A infection: On alert for outbreaks. Nursing, 48(4), 66–69. https://doi.org/10.1097/01.NURSE.0000531014.78460.95